What is erythremia
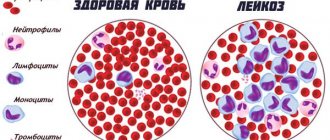
With erythremia, proliferation (growth) of red blood cells occurs and the number of other cells greatly increases (pancytosis). There is also an increase in hemoglobin.
Is erythremia an oncology, is it cancer or not? Most often, erythremia is benign in nature, with a long course, but degeneration of the benign form of the disease into a malignant one can occur, followed by death.
Erythremia is a fairly rare disease. It is diagnosed in approximately 4 out of 100 million people per year. The disease does not depend on the gender of the person, but usually develops in patients after 50. At a young age, cases of the disease are more often diagnosed in women. Erythremia (ICD 10 code - C 94.1) is characterized by a chronic form of the course.
For your information! Erythremia is considered one of the most benign blood diseases. Death often occurs due to the progression of various complications.
The disease is asymptomatic for a long time. Patients with this diagnosis tend to bleed heavily (although the level of platelets, which are responsible for stopping bleeding, is elevated).
There are two types of erythremia: acute form (erythroleukemia, erythromyelosis, erythroleukemia) and chronic. Depending on the progression, they are divided into true and false. The first form is characterized by a persistent increase in the number of blood cells and is extremely rare in children. The peculiarity of the second type is that the level of red blood cells is normal, but the plasma volume is slowly decreasing. Depending on the pathogenesis, the true form is divided into primary and secondary (erythrocytosis).
Symptomatic manifestations
Pain in the liver area is one of the symptoms of erythremia
Unlike the causes, the signs of erythremia have been studied very well. Most often, the patient experiences the following symptoms:
- Fatigue (feeling “like unloading a train of coal”);
- Performance is reduced;
- Sweat is released more often and more abundantly than usual;
- My head hurts a lot and I feel dizzy;
- Memory problems;
- Hearing decreases.
- Vision deteriorates;
- There is pain in the fingers (“they sprinkled pepper”);
- The limbs themselves also hurt;
- The body itches, especially if you take a shower or a hot bath;
- Rashes appear on the skin every now and then (similar to hives). Heart ache;
- Since platelets along with red blood cells accumulate and are then destroyed in the liver, it enlarges, so pain is felt in this area;
- The spleen also enlarges;
- A stomach ulcer begins to form;
- It becomes difficult to urinate;
- Uric acid diathesis develops, causing pain in the waist area;
- The bone marrow grows (hyperplasia). This leads to gout and joint pain;
- Vessels in the conjunctiva may burst, causing the eyes to become visually red;
- Thrombosis begins in the arteries and veins;
- Varicose veins may also appear;
- The person begins to noticeably limp.
Red face due to erythremia
Since the immune system weakens significantly, infections easily penetrate the body. The respiratory organs are the first to be attacked. As soon as the immune system begins to react to microbes, red blood cells suppress this reaction. Changes also occur in the central nervous system (insomnia).
Important! A person may not even know that they have erythremia because the disease develops slowly.
Over time, plethora manifests itself as swollen veins, cherry-colored skin, and red eyes. Cooperman's symptom occurs - the soft palate has one color, the hard palate has the usual color. This is due to slower blood circulation.
How does erythremia develop?
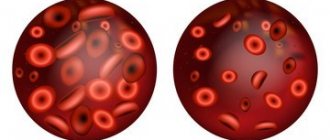
Erythremia develops as follows. Red blood cells (their function is to deliver oxygen to all cells of the human body) begin to be intensively produced so that they cannot fit into the bloodstream. When these red blood cells overwhelm the bloodstream, blood viscosity and blood clot formation increase. Hypoxia increases, cells do not receive enough nutrition, and the entire functioning of the body begins to malfunction.
Where are red blood cells formed in the human body? Red blood cells are formed in the red bone marrow, liver, and spleen. The distinctive ability of red blood cells is the ability to divide, transforming into another cell.
The normal level of hemoglobin in the blood is different and depends on age and gender (in children and older people its amount is lower). The normal content of red blood cells (normocytosis) in 1 liter of blood is:
- for men – 4.0 – 5.0 x 1012;
- for women – 3.5 – 4.7 x 1012.
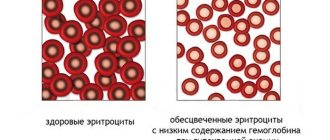
The cytoplasm of an erythrocyte is almost 100% occupied by hemoglobin, which contains an iron atom. Hemoglobin gives the red color to red blood cells and is responsible for the delivery of oxygen to all organs and the removal of carbon dioxide.
The formation of red blood cells is constant and continuous, starting from intrauterine development (in the third week of embryo formation) and until the end of life.
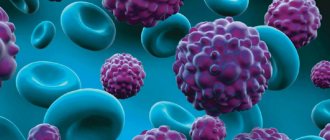
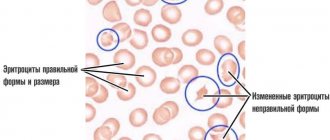
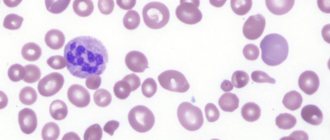
As a result of mutations, a pathological clone of a cell is formed, which has similar capabilities for modification (can become an erythrocyte, platelet or leukocyte), but is not under the control of the body’s regulatory systems that maintain the cellular composition of the blood. The mutant cell begins to multiply, and the result of this is the appearance of absolutely normal red blood cells in the blood.
This is how 2 different types of cells arise - normal and mutant. As a result, the number of mutated cells in the blood increases, exceeding the body's needs. This inhibits the release of erythropoietin by the kidneys and leads to a decrease in its effect on the normal process of erythropoiesis, but does not affect the tumor cell. As the disease progresses, the number of mutant cells increases and they displace normal cells. There comes a moment when all the red blood cells in the body arise from the tumor cell.
With erythremia, a maximum of mutant cells turn into nuclear charged erythrocytes (erythrokaryocytes), but a certain part of them develops with the formation of platelets or leukocytes. This explains the increase in the number of not only red blood cells, but also other cells. Over time, the level of platelets and white blood cells obtained from the cancer cell increases. The process of sludge occurs—the blurring of the boundaries between red blood cells. But the erythrocyte membrane is preserved, and sludge is a pronounced aggregation - crowding of erythrocytes. Aggregation leads to a sharp increase in blood viscosity and a decrease in its fluidity.
Causes of erythremia
There are some factors that contribute to the occurrence of erythremia:
- genetic predisposition . If there is a patient in the family, the risk of developing it in one of the relatives increases. The risk of developing the disease also increases if a person has: Down syndrome, Klinefelter syndrome, Bloom syndrome, Marfan syndrome. The predisposition to erythremia is explained by the instability of the genetic cellular apparatus, because of this a person becomes susceptible to negative external influences - toxins, radiation;
- ionizing radiation . X-rays and gamma rays are partially absorbed by the body, affecting genetic cells. But the strongest radiation is experienced by people who are being treated for cancer with chemotherapy, and those who were at the epicenter of power plant explosions and atomic bombs;
- toxic substances found in the body. When they enter the body, they can contribute to the mutation of genetic cells; such substances are called chemical mutagens. These include: cytostatic drugs (antitumor drugs - Azathioprine, Cyclophosphamide), antibacterial drugs (Levomycetin), benzene.
Development factors
Although no cause has been identified, there are several factors that increase the risk of developing the disease. These include:
- Down syndrome is a genetic disease characterized by a disproportionate shape of the face, neck and head, as well as mental retardation.
- Bloom's syndrome - with this genetic disease, short stature, excessive pigmentation of the skin and a tendency to form tumors are observed.
- Klinefelter syndrome is a male genetic pathology that is detected only at the onset of puberty; characterized by excessive growth and length of limbs, developmental problems are possible.
- Marfan syndrome is a genetic disease that affects connective tissue, causing high growth, excessive length of limbs, problems with vision and the cardiovascular system.
- Ionizing radiation (including uncontrolled use of X-ray diagnostics).
- Use of chemical mutagens (some cytostatics, antibiotics, etc.) in treatment.
Stages of the disease and symptoms of erythremia
Erythremia is a long-term disease. Its beginning is hardly noticeable. Sufferers often live for decades with minor symptoms. But in more serious cases, due to the formation of blood clots, death can occur within 4-5 years. Along with the development of erythremia, the spleen grows. There is a form of the disease with cirrhosis of the liver and damage to the diencephalon. The disease may involve allergic and infectious complications; often patients cannot tolerate certain medications and suffer from urticaria and other skin diseases.
Course and outcomes
The course of erythremia is chronic, steadily progressing. The average duration of an untreated disease is from 8 to 10 years.
There are three phases of the disease:
• initial (prodromal);
• erythremic (polycythemic);
• terminal (outcome phase).
The initial phase is characterized by slight erythrocytosis (5-6 million) and the absence of pronounced leukocytosis and thrombocytosis. The disease in this phase is almost asymptomatic.
The erythremic phase eventually passes into the third - terminal phase of the disease, which in turn is heterogeneous.
It is necessary to distinguish:
• Outcomes associated with organ and vascular pathology in erythremia: liver cirrhosis, coronary thrombosis, softening areas in the brain due to thrombosis and hemorrhage, etc.
• “Hematological” outcomes due to the very essence of erythremia, which is a disease of the hematopoietic system. Of these, the main outcomes are anemia and myeloid leukemia.
The transformation of erythremia into anemia is based on the gradual development of myelofibrosis and osteomyelosclerosis. The development of severe myelofibrosis syndrome is preceded by the stage of myeloid metaplasia of the spleen. The latter occurs in the erythremic phase, when the bone marrow is still sharply hyperplastic.
The development of myelofibrosis with erythremia is accompanied by a gradual enlargement of the spleen and liver due to myeloid metaplasia. Myeloid metaplasia of the spleen and liver is an expression of the myeloproliferative, systemic nature of the disease. At the same time, extramedullary foci of hematopoiesis that arise against the background of progressive myelofibrosis have a known compensatory value. With the development of myelofibrosis, external signs of erythremia gradually disappear. Red blood counts return to normal and remain at this level sometimes for several years; then anemia develops. The number of leukocytes ranges from leukopenic to subleukemic numbers. The content of band and segmented neutrophils is always sharply increased, there is a moderate shift to myelocytes, less often - myeloblasts. Normoblastosis, polychromasia, and basophilic punctation of erythrocytes appear.
The diagnosis of myelofibrosis is established on the basis of a bone marrow biopsy and puncture of the spleen and liver.
Another line of development of erythremia is the outcome of acute and chronic myeloid leukemia.
Acute myeloid leukemia is the cause of death in patients with erythremia in 10-20% of cases.
Diagnosis of erythremia
To diagnose erythremia, the most important test is a general blood test (CBC). Deviations of these laboratory parameters relative to the norm become the first sign of the disease. At the very beginning, blood counts do not differ much from the norm, but as the disease progresses, they increase, and at the last stage they fall.
If erythremia is diagnosed, blood counts indicate an increase in red blood cells and hemoglobin. The hematocrit, which indicates the blood's ability to carry oxygen, rises to 60-80%. Platelets and leukocytes are increased. A diagnosis cannot be made on the basis of the CBC alone. In addition to a general blood test, the following is performed:
- blood chemistry. It detects the iron content in the blood and the value of liver tests (AST and ALT). The level of bilirubin indicates the severity of the process of destruction of red blood cells;
- bone marrow puncture. This analysis shows the state of hematopoietic cells in the bone marrow - their number, the presence of tumor cells and fibrosis;
- Ultrasound of the abdominal cavity. This examination helps to see the overflow of organs with blood, the growth of the liver and spleen, and areas of fibrosis;
- Dopplerography. Detects the presence of blood clots and shows the speed of blood movement.
Also, when diagnosing erythremia, the level of erythropoietin is determined. This study determines the state of the hematopoietic system and indicates the level of red blood cells in the blood.
Would you like to receive an estimate for treatment?
*Only upon receipt of data on the patient’s disease, a representative of the clinic will be able to calculate an accurate estimate for treatment.
Diagnosis and differential diagnosis
Currently, due to the advent of effective treatments for erythremia, the importance of the differential diagnosis of erythremia has increased significantly. It is necessary to clearly differentiate erythremia from a large group of erythrocytoses, which have nothing in common with erythremia except external similarity in the form of an increase in the number of red blood cells.
Erythremia is supported by a high degree of erythrocytosis, leukocytosis, and in the absence of the latter, noticeable and persistent neutrophilia and a band shift in the blood count, as well as thrombocytosis. Hypoxic erythrocytosis is characterized by an increase in the volume of red blood cells.
Splenomegaly is characteristic of erythremia and is usually absent in erythrocytosis.
A hematocrit value above 70/30 is more typical for erythremia. With erythrocytosis, a moderate increase in hematocrit may occur.
Determining the mass of erythrocytes helps to differentiate erythremia from relative erythrocytosis, as well as from absolute (secondary) erythrocytosis, in which the mass of erythrocytes, although increased, is to a much lesser extent than with erythremia.
A decrease in the oxygen content in arterial blood is characteristic of hypoxic erythrocytosis and does not occur with erythremia. A very significant differential diagnostic feature is bone marrow megakaryocytosis in erythremia.
Most likely, an early and differential diagnosis of erythremia is established on the basis of a histological examination of bone marrow obtained by trepanobiopsy. Erythremia is characterized by pronounced hyperplasia of the cellular elements of the bone marrow, leading to almost complete displacement of fat, and especially megakaryocytosis. In secondary erythrocytosis, megakaryocytosis is usually absent, hyperplasia of cellular elements is absent or very small. The simplicity and safety of this research method allow us to recommend it for the differential diagnosis of erythremia in all unclear cases.
Treatment of erythremia
Polycythemia progresses slowly. At the first stage of polycythemia, the main goal of treatment is to reduce blood counts to normal: hemoglobin and red blood cell hematocrit. It is also important to minimize complications caused by erythremia. To normalize hematocrit with hemoglobin, bloodletting is used. There is a procedure called erythrocytapheresis, which refers to the purification of red blood cells from the blood. The blood plasma is preserved.
Drug treatment includes the use of cytostatics (antitumor drugs) that help with complications (thrombosis, ulcers, cerebral circulatory disorders). These include Myelosan, Busulfa, Imifos, hydroxyurea, radioactive phosphorus.
For hemolytic anemia of autoimmune origin, glucocorticosteroids are used - Prednisolone. If such therapy does not have an effect, surgery is performed to remove the spleen.
To avoid iron deficiency, iron-containing drugs are prescribed - “Maltofer”, “Hemofer”, “Sorbifer”, “Totema”, “Ferrum Lek”.
If necessary, the following groups of drugs are prescribed:
- lowering blood pressure - “Lisinopril”, “Amlodipine”;
- antihistamines – “Periaktin”;
- blood thinners (anticoagulants) - “Aspirin”, “Curantil” (“Dipyridamole”), “Heparin”;
- improving heart function - “Korglikon”, “Strofanthin”;
- to prevent the development of stomach ulcers - gastroprotectors - “Almagel”, “Omeprazole”.
Diet for erythremia and folk remedies
To combat the disease, the patient should follow a plant-based and fermented milk diet. Proper nutrition includes eating foods such as:
- vegetables - raw, boiled, stewed;
- kefir, cottage cheese, milk, yogurt, sourdough, yogurt, fermented baked milk, sour cream;
- eggs;
- tofu and brown rice dishes;
- whole wheat bread;
- greens (spinach, dill, sorrel, parsley);
- almond;
- dried apricots and grapes;
- tea (preferably green).
Red vegetables and fruits and their juices, soda, sweets, fast food, and smoked foods are contraindicated. You should limit the amount of meat you consume.
To prevent the appearance of blood clots at stage 2 of the disease, drink juice made from horse chestnut flowers.
To normalize blood pressure and for migraines, it is recommended to use an infusion of medicinal clover. The course should be limited to 10-14 days.
To dilate blood vessels, improve blood flow, and increase the resistance of capillaries and blood vessels, it is recommended to use decoctions of mushroom herbs, periwinkle, nettle, and burial ground.
Nutritional Features
Dietary nutrition is one of the important elements of medical procedures. The diet for erythremia is aimed at thinning the blood and minimizing the production of red blood cells, which has a positive effect on the patient’s condition.
Regardless of the stage of the disease, doctors recommend refraining from consuming:
- Alcohol, which destroys tissues and organs.
- Fruit and vegetable dishes (based on red fruits).
- Foods rich in preservatives and dyes.
- Beef, liver.
- Fish dishes.
- Products rich in ascorbic acid (with high hemoglobin blood levels).
- Simple (refined) carbohydrates.
The diet is allowed to include:
- Whole grain products.
- Eggs.
- Dairy products (low fat).
- White beans.
- Greenery.
- Nuts.
- Green tea.
- Raisins, dried apricots (in limited quantities).
The recommended frequency of meals for erythremia is 4-6 times a day (in small portions). The daily consumption rate of purified water, which thins the blood, is at least 2 liters.
https://youtu.be/Lcjs_PZOOA0
Disease prognosis
Erythremia is considered a benign disease, but without adequate treatment it can be fatal.
The prognosis of the disease depends on several factors:
- timely diagnosis of the disease - the earlier the disease is detected, the sooner treatment will begin;
- correctly prescribed treatment;
- the level of leukocytes, platelets and red blood cells in the blood - the higher their level, the worse the prognosis;
- the body's response to treatment. Sometimes, despite treatment, the disease progresses;
- thrombotic complications;
- rate of malignant tumor transformation.
In general, the prognosis for life with erythremia is positive. With timely diagnosis and treatment, patients can live more than 20 years from the moment the disease is detected.