What it is?
AML is a malignant transformation involving the myeloid lineage of blood cells.
Affected blood cells gradually replace healthy ones, and the blood ceases to fully perform its work.
This disease, like other types of leukemia, is called blood cancer in everyday conversation.
The words that make up this definition make it possible to understand it better.
Leukemia. With leukemia, the altered bone marrow begins to actively produce leukocytes - blood elements that are responsible for maintaining the immune system - with a pathological, malignant structure.
They replace healthy leukocytes , penetrate into different parts of the body and form lesions there, similar to malignant neoplasms.
Differences between healthy blood and leukemia patients
Myeloblastic. With AML, excessive production of affected myeloblasts begins - elements that should turn into one of the types of leukocytes.
They crowd out healthy precursor elements , leading to a deficiency of other blood cells: platelets, red blood cells, and normal white blood cells.
Spicy. This definition suggests that it is immature elements that are produced. If the affected cells are in a mature state, leukemia is called chronic.
Acute myeloblastosis is characterized by rapid progression: myeloblasts in the blood spread throughout the body and cause tissue infiltration.
Leukemia
Stages of myeloid leukemia and symptoms
Blood cancer goes through three stages in its development:
- Chronic, in which the patient does not experience any symptoms. The disease occurs in a latent form. Malaise and weakness are felt by the sick person as symptoms of fatigue. As the pathological condition develops, the patient begins to lose weight and loses his appetite. Pain appears in the left side of the abdomen, especially after eating. It indicates an enlarged spleen. In rare cases, these symptoms may be accompanied by blurred vision, shortness of breath, and bleeding.
- Acceleration, during which all the symptoms of the chronic stage become aggravated and increase. In this phase, there is a loss of strength, profuse sweating, and an unreasonable increase in temperature to 38-39 degrees. A person is constantly losing weight, he is tormented by endless pain in the left hypochondrium. An enlarged spleen can be felt independently. At the acceleration stage, damage to the cardiovascular system occurs, which will be expressed in frequent heart attacks and arrhythmias.
- The terminal (last) stage of myeloid leukemia, in which the patient’s condition sharply worsens. He feels intolerable pain in the bones, which is the result of damage to malignant cells of the red bone marrow. Weight loss continues and fever persists. Bruises and bruises appear on the body, because... platelet count decreases. Due to the intense increase in the size of the spleen, a feeling of heaviness, pain and fullness appears in the abdomen. During this time, patients are very susceptible to various infectious diseases, which can cause their death.
Symptoms
AML usually develops in adults and older people. The early stages of myeloid leukemia are characterized by the absence of pronounced symptoms, but when the disease has taken hold of the body, serious impairments of many functions occur.
Hyperplastic syndrome
Develops due to tissue infiltration under the influence of leukemia. Peripheral lymph nodes grow , the spleen, palatine tonsils, and liver enlarge.
The lymph nodes of the mediastinal region are affected: if they grow significantly, they compress the superior vena cava.
The blood flow in it is disrupted , which is accompanied by swelling in the neck area, rapid breathing, bluishness of the skin, and swelling of blood vessels in the neck.
The gums are also affected : Vincent's stomatitis appears, which is characterized by the development of severe symptoms: the gums swell, bleed and are very painful, it is difficult to eat and take care of the oral cavity.
Hemorrhagic syndrome
More than half of the patients have one or another of its manifestations; it develops due to an acute lack of platelets, in which the walls of blood vessels become thinner, blood clotting is impaired: multiple bleedings are observed - nasal, internal, subcutaneous, which cannot be stopped for a long time.
The risk of hemorrhagic stroke increases - a cerebral hemorrhage, in which the mortality rate is 70-80%.
In the early stages of acute myeloid leukemia, a bleeding disorder manifests itself in the form of frequent nosebleeds, bleeding gums, and bruises on different parts of the body that appear from minor impacts.
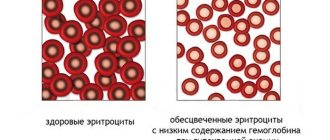
Anemia
Characterized by the appearance of:
- Marked weakness
- Fatigue,
- Deterioration in working capacity,
- Irritability,
- Apathy,
- Frequent headaches
- Dizziness,
- Fainting,
- Aspirations are chalk,
- drowsiness,
- Pain in the heart area,
- Pale skin.
Even minor physical activity is difficult (severe weakness, rapid breathing are observed). With anemia, hair often falls out and nails become brittle.
Intoxication
The body temperature is elevated, weight falls, appetite disappears, weakness and excessive sweating are observed.
The initial manifestations of intoxication are observed in the initial stages of the development of the disease.
Neuroleukemia
If infiltration affects brain tissue, this worsens the prognosis.
The following symptoms are observed:
- Repeated vomiting
- Acute pain in the head
- Seizures,
- Fainting,
- Intracranial hypertension,
- Failures in perception of reality,
- Hearing, speech and vision impairments.
Leukostasis
They develop in the later stages of the disease, when the number of affected myeloblasts in the blood becomes above 100,000 1/μl.
The blood thickens , the blood flow becomes slow, and blood circulation in many organs is disrupted.
Cerebral leukostasis is characterized by the occurrence of intracerebral bleeding . Vision is impaired, a stuporous state, coma occurs, and death is possible.
With pulmonary leukostasis, rapid breathing is observed (tachypnea may occur), chills, and fever. The amount of oxygen in the blood decreases.
In acute myeloid leukemia, the immune system is extremely vulnerable and is unable to protect the body, therefore there is a high susceptibility to infections, which are severe and have a lot of dangerous complications.
Kinds
Myeloid leukemia in medicine is divided into two types:
- chronic myeloid leukemia (the most common form);
- acute myeloid leukemia.
Acute myeloid leukemia
Acute myeloid leukemia
Acute myeloid leukemia is a blood disease in which uncontrolled proliferation of white blood cells occurs. Full-fledged cells are replaced with leukemic ones. The pathology is fast-acting and without adequate treatment a person may die within a few months. The patient’s life expectancy directly depends on the stage at which the presence of the pathological process is detected. Therefore, it is important, if you have the first symptoms of myeloid leukemia, to contact a qualified specialist who will conduct a diagnosis (the most informative is a blood test), confirm or refute the diagnosis. Acute myeloid leukemia affects people from different age groups, but most often it affects people over 40 years of age.
Acute symptoms
Symptoms of the disease usually appear almost immediately. In very rare clinical situations, the patient's condition worsens gradually.
- nosebleeds;
- hematomas that form over the entire surface of the body (one of the most important symptoms for diagnosing pathology);
- hyperplastic gingivitis;
- night sweats;
- ossalgia;
- shortness of breath appears even with minor physical exertion;
- a person often falls ill with infectious diseases;
- the skin is pale, which indicates a disorder of hematopoiesis (this symptom is one of the first to appear);
- the patient's body weight gradually decreases;
- petechial rashes are localized on the skin;
- temperature rise to subfebrile level.
If you have one or more of these symptoms, it is recommended to visit a medical facility as soon as possible. It is important to remember that the prognosis of the disease, as well as the life expectancy of the patient in whom it is detected, largely depends on timely diagnosis and treatment.
Chronic myeloid leukemia
Chronic myeloid leukemia is a malignant disease that exclusively affects hematopoietic stem cells. Gene mutations occur in immature myeloid cells, which in turn produce red blood cells, platelets, and virtually all types of white blood cells. As a result, an abnormal gene called BCR-ABL is formed in the body, which is extremely dangerous. It “attacks” healthy blood cells and converts them into leukemia cells. Their location is the bone marrow. From there, they spread through the bloodstream throughout the body and affect vital organs. Chronic myeloid leukemia does not develop rapidly; it is characterized by a long and measured course. But the main danger is that without proper treatment it can develop into acute myeloid leukemia, which can kill a person in a few months.
The disease in most clinical situations affects people from various age groups. In children, it occurs sporadically (cases of morbidity are very rare).
Chronic myeloid leukemia occurs in several stages:
- chronic. Leukocytosis increases gradually (it can be detected using a blood test). Along with it, the level of granulocytes and platelets increases. Splenomegaly also develops. At first, the disease may be asymptomatic. Later, the patient develops rapid fatigue, sweating, and a feeling of heaviness under the left rib, caused by an enlarged spleen. As a rule, a patient turns to a specialist only after he experiences shortness of breath during minor exertion or heaviness in the epigastrium after eating. If you conduct an X-ray examination at this moment, the image will clearly show that the dome of the diaphragm is lifted upward, the left lung is pushed back and partially compressed, and the stomach is also compressed due to the enormous size of the spleen. The most terrible complication of this condition is splenic infarction. Symptoms: pain on the left under the rib, radiating to the back, fever, general intoxication of the body. At this time, the spleen is very painful on palpation. Blood viscosity increases, which causes veno-occlusive liver damage;
- acceleration stage. At this stage, chronic myeloid leukemia practically does not manifest itself or its symptoms are expressed to an insignificant extent. The patient's condition is stable; sometimes there is an increase in body temperature. A person gets tired quickly. The level of leukocytes increases, and metamyelocytes and myelocytes also increase. If you conduct a thorough blood test, you will find blast cells and promyelocytes in it, which should not normally be present. The level of basophils increases up to 30%. As soon as this happens, patients begin to complain of skin itching and a feeling of heat. All this is due to an increase in the amount of histamine. After additional tests have been performed (the results of which are placed in the medical history to observe trends), the dose of the chemical is increased. a drug used to treat myeloid leukemia;
- terminal stage. This stage of the disease begins with the appearance of joint pain, severe weakness and an increase in temperature to high numbers (39–40 degrees). The patient's weight decreases. A characteristic symptom for this stage is splenic infarction due to its excessive enlargement. The man is in very serious condition. He develops hemorrhagic syndrome and blast crisis. More than 50% of people are diagnosed with bone marrow fibrosis at this stage. Additional symptoms: enlarged peripheral lymph nodes, thrombocytopenia (detected by a blood test), normochromic anemia, the central nervous system is affected (paresis, nerve infiltration). The patient's life expectancy depends entirely on supportive drug therapy.
Causes
The exact causes of AML are unknown, but there are a number of factors that increase the likelihood of developing the disease:
- Radiation exposure. At risk are people who interact with radioactive materials and devices, liquidators of the consequences of the Chernobyl Nuclear Power Plant, and patients undergoing radiation therapy for another cancer.
- Genetic diseases. With Faconi anemia, Bloom and Down syndromes, the risk of developing leukemia increases.
- Exposure to chemicals. Chemotherapy in the treatment of malignant diseases negatively affects the bone marrow. The likelihood also increases with chronic poisoning by toxic substances (mercury, lead, benzene and others).
- Heredity. People whose close relatives suffered from leukemia may also become ill.
- Myelodysplastic and myeloproliferative syndromes. If one of these syndromes is not treated, the disease can transform into leukemia.
This type of leukemia is extremely rarely diagnosed in children; people over 50-60 years of age are at risk.
Forms and causes of AML
Depending on the stage at which the stem cell has mutated, different types of myeloid leukemia are distinguished:
- with or without ripening;
- myelomonocytic;
- monoblastic (monocyte);
- erythroblastic;
- megakaryoblastic;
- basophilic;
- eosinophilic and other myeloblastic leukemias.
AML with minimal differentiation and mixed type leukemia are also distinguished.
Currently, there is a tendency to determine the form of myeloid leukemia not by the type of cells into which blasts would develop, but by the types of genetic mutations in malignant cells. Based on this trend, myeloid leukemia is classified based on this feature.
Important: do not confuse acute myeloblastic leukemia with multiple myeloma. Multiple myeloma is a paraproteinemic form of leukemia, which, in turn, is part of the group of chronic lymphocytic leukemias.
The causes of AML in children and adults are not known with certainty. Risk factors are:
- genetic cell mutations inherited;
- some chromosomal diseases;
- congenital or acquired immunodeficiency;
- exposure to radiation, ultraviolet radiation, various carcinogens, taking certain medications - cytostatics, alkylating agents, drugs containing arsenic, and some others.
In addition to the above circumstances, theories about the relationship between the occurrence of myeloblastic blood cancer and some viral diseases, as well as bad habits, are currently under question.
It is believed that the likelihood of developing AML is particularly high in patients whose body functioning is influenced by several of the factors mentioned.
Forms of AML
Myeloblastic leukemia has a number of varieties, which determine the prognosis and treatment tactics.
| Name and FAB classification | Description |
| AML with slight differentiation (M0). | Low susceptibility to chemotherapy treatment, easily acquires resistance to it. The prognosis is unfavorable. |
| AML without maturation (M1). | It is characterized by rapid progression, blast cells are contained in large numbers and make up about 90%. |
| AML with maturation (M2). | The level of monocytes in this variety is less than 20%. At least 10% of myeloblastic elements develop to the promyelocyte stage. |
| Promyelocytic leukemia (M3). | Promyelocytes accumulate intensively in the bone marrow. It is one of the most favorable leukemias in terms of course and prognosis - at least 70% live for 10-12 years. Symptoms are similar to other types of AML. It is treated with arsenic oxide and tretinoin. The average age of patients is 30-45 years. |
| Myelomonocytic leukemia (M4). | It is diagnosed in children more often than other types of the disease (but in general, AML as a percentage, compared to other types of leukemia, is rarely detected in children). It is treated with intensive chemotherapy and stem cell transplant (SCT). The prognosis is unfavorable - survival rates for five years are 30-50%. |
| Monoblastic leukemia (M5). | With this type, the bone marrow contains at least 20-25% blast elements. Treated with chemotherapy and THC. |
| Erythroid leukemia (M6). | Rarely found variety. It is treated with chemotherapy and stem cell transplantation. The prognosis is unfavorable. |
| Megakaryoblastic leukemia (M7). | This type of AML affects people with Down syndrome. It is characterized by a rapid course and low susceptibility to chemotherapy. Childhood forms of the disease often progress favorably. |
| Basophilic leukemia (M8). | It is more common in childhood and adolescence; the life prognosis for M8 is unfavorable. In addition to malignant elements, abnormal elements are detected in the blood, which are difficult to identify without special equipment. |
Also, in addition to the varieties mentioned, there are other rare species that are not included in the general classification.
Causes and mechanisms of development
Acute myeloid leukemia (AML), like any leukemia, arises from a single mutated cell that loses its ability to mature and begins to multiply uncontrollably. It is usually impossible to say exactly which of the known carcinogenic factors provoked mutations in each specific case, especially when it comes to children. In general these could be:
- Biological factors: oncogenic viruses, the most famous of which is Epstein-Bar.
- Chemical substances. In total, more than one and a half thousand carcinogenic compounds are known. These include: products of incomplete combustion of tobacco; substances arising from incomplete oxidation of fats (deep frying); industrial “hazards” that appear during the thermal treatment of oil, resins, and coal; mold waste products; medications used for chemotherapy of malignant tumors (sadly, there are cases when leukemia occurs 10-20 years after successful removal of cancer).
- Physical factors. This is mainly ionizing or x-ray radiation: it is known that for X-ray room workers the likelihood of getting sick is higher than the average for the population.
In addition to external influences, heredity matters: it is known, for example, “leukemia of twins,” or passed on in the family from generation to generation. It is not the disease itself that is inherited, but gene or chromosomal mutations that increase its likelihood. In addition, some congenital pathologies are combined with a higher incidence of leukemia, in particular myeloid leukemia:
- Down syndrome;
- neurofibromatosis type 2;
- Falconi's anemia;
- severe congenital anemia;
- congenital thrombocytopenia or thrombocytopathy.
The pathogenesis, or development mechanism, of myeloblastic leukemia is based on competition between normal and tumor cells. Initially, one single atypical cell in 3 months is capable of generating 1012 - one trillion - daughter blasts, with a total mass of more than a kilogram. Malignant cells live longer because their mechanism of “aging” and natural death is turned off. They produce substances that inhibit the activity of healthy blood elements and suppress growth factors. In such a situation, the possibilities of normal hematopoiesis are gradually depleted.
In addition, the body, “seeing” a huge number of myeloblasts in the bone marrow and vascular bed, begins to slow down the activity of hematopoiesis: since all cells are somehow differentiated from blast cells, it perceives degenerative, malignant cells as “normal”. This is another mechanism that allows oncology to win the competition. As hemoblastosis develops, malignant cells begin to multiply in other tissues and organs: liver, spleen, lymph nodes, skin and even meninges.
It is the replacement of healthy blood cells with a mass of blasts, unable to perform their functions due to immaturity, that forms the symptoms of leukemia.
Diagnostics
Acute leukemia is detected using a number of diagnostic measures.
Diagnostics includes:
- Detailed blood test. With its help, the content of blast elements in the blood and the level of other blood cells are detected. With leukemia, an excess number of blasts and a reduced content of platelets, mature leukocytes, and erythrocytes are detected.
- Taking biomaterial from the bone marrow. It is used to confirm the diagnosis and is carried out after blood tests have been performed. This method is used not only during the diagnostic process, but also throughout treatment.
- Biochemical analysis. Provides information about the condition of organs and tissues, the content of various enzymes. This analysis is prescribed to obtain a detailed picture of the lesion.
- Other types of diagnostics : cytochemical study, genetic, ultrasound of the spleen, abdominal cavity and liver, x-ray of the chest area, diagnostic measures to determine the extent of brain damage.
Other diagnostic methods may be prescribed, depending on the patient’s condition.
Diagnosis and tests for myeloid leukemia
If myeloid leukemia is suspected, the patient is asked to undergo a series of studies - ultrasound diagnostics of the abdominal organs and laboratory blood tests:
- General blood analysis.
- Red bone marrow biopsy.
- Blood PCR.
- Cytogenetic blood test.
Ultrasound of the abdominal organs
At the chronic stage of the disease, the spleen increases in size. At the acceleration stage, ultrasound of the spleen and liver shows their increase by more than 10 cm, and during blast crisis the spleen reaches enormous sizes - it occupies almost the entire abdominal cavity. Her weight ranges from 5-8 kg.
Preparation for ultrasound examination of the abdominal organs is carried out on an empty stomach. You should also not drink water at least 4 hours before the procedure. 2 days before this, all foods that can lead to gas formation, as well as alcoholic beverages, are excluded from the menu. Patients suffering from constipation are recommended to undergo a cleansing enema. You should not smoke before an ultrasound.
The patient receives the results of the study immediately after the procedure.
General blood analysis
When a patient comes to the doctor with complaints of general malaise, headaches and fatigue, the doctor sends him for a general blood test, which is very effective and indicative of many diseases. Despite the fact that they have many indicators, it is impossible to make a diagnosis with just this study.
The test is taken in the morning, on an empty stomach. It is necessary to exclude the consumption of fatty foods during the day, because this may skew the results. Capillary blood from the fingertip is used as a biological material. Usually the result is ready within a few hours.
At the chronic stage, only a general blood test can recognize the disease, which shows, in the presence of a pathological process, an increase in immature blood cells, basophils (more than 0.1%), eosinophils (more than 5%) and a serious increase in leukocytes (more than 9 thousand) and a decrease in platelets without special reasons (in an adult - less than 180, in children over the age of one year - less than 160).
At the acceleration stage, a general blood test shows:
- the number of myeloblasts increases to 20% - a healthy person should not have them in the blood;
- the number of basophils increases to 20%
- The platelet level decreases to 100 thousand units;
- the number of leukocytes continues to increase.
At the terminal stage, a general blood test indicates:
- an increase in the number of myelo and lymphoblasts by 20 percent or more;
- about the appearance of large accumulations of blasts in the bone marrow.
These are immature blood cells that are later converted into blood cells. In the absence of pathology in the blood, they do not occur. Therefore, when blasts are detected in the blood, the bone marrow is also checked for their presence.
Study of red bone marrow in myeloblastic leukemia
Blood cells are produced by red bone marrow. In order to confirm the diagnosis, a red bone marrow puncture is performed and a part of the bone is sent for examination. Most often, a biopsy is taken from the sternum, pelvis (in adults), and calcaneus (in children under 2 years of age).
Under local anesthesia, the doctor pierces the bone with a special syringe and needle - in adults at a depth of 3-4 cm, in children - 1-2 cm - and draws tissue from the bone cavity into the syringe. Then the resulting biomaterial is applied to glass and studied under a microscope in the laboratory.
Preparation for the procedure will consist of the following: a conversation is held with the doctor about the presence of an allergic reaction to the anesthetic. In addition, a patient taking blood thinners is advised to abstain from them for 2 weeks.
On the eve of the puncture, the patient needs to cleanse the intestines and bladder, take a shower, and the man needs to remove the hair on the chest at the puncture site. The patient is given a sedative and an anesthetic 30 minutes later. After this, the doctor pierces the soft tissue in the area of the bone, feels it and inserts a needle and syringe there, collecting biomaterial. After this, the puncture site is treated with an antiseptic. The procedure time is 20-30 minutes. Studying a sample takes from 2 to 4 hours, in some cases - in the absence of your own laboratory - it can take up to a month to get the result.
The patient can go home after 30 minutes. For 3 days you should not shower or bathe so as not to wet the puncture site.
Puncture of the red brain is not performed in the following cases:
- in acute myocardial infarction;
- in case of acute cerebrovascular accident;
- during hypertensive crisis;
- during an attack of angina.
Chronic myeloid leukemia is indicated in the analysis results by the number of leukocytes, above 17 in adults and more than 35% in children after 5 years. If the number of blasts (erythroblasts, normoblasts) is increased by 20%, we are talking about acute leukemia.
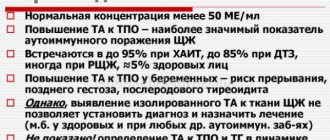
PCR for the presence of the BCR gene - ABL1
The polymerase chain reaction method makes it possible to accurately determine not only the presence of viruses, but also chromosomal abnormalities. PCR is aimed at searching for the BCR gene - ABL1, which causes blood cancer. This is a very complex chemical process that requires special laboratory conditions and highly qualified professionals.
For analysis, venous blood or red bone marrow is taken. If a blood test is required, venous blood is taken from the patient in the morning on an empty stomach. For the reliability of the analysis, it is recommended not to use medications 2 weeks before the analysis. The results are prepared within 24 hours. If the BCR - ABL1 gene is detected, even in small quantities, then the diagnosis of chronic myeloid leukemia is confirmed.
Cytogenetic study for the presence of Ph Philadelphia chromosome
The presence of the Philadelphia chromosome confirms the diagnosis of myeloblastic leukemia. This chromosome appears as a result of the union of two sections on the 22nd chromosome. Ph search is carried out using the PCR method discussed above.
This chromosomal abnormality is observed in 95% of cases of the chronic stage of the disease, which means this method helps to identify the disease at an early stage.
Treatment
Treatment of AML includes the use of the following methods:
- Chemotherapy. Medicines act on cells, suppressing their activity and reproduction. A key treatment for leukemia.
- Consolidation. Treatment given during remission is aimed at reducing the likelihood of relapse.
- Stem cell transplantation. Bone marrow transplantation for leukemia is used in the treatment of patients under 25-30 years of age and is necessary in situations where the disease course is unfavorable (neuroleukemia is observed, the concentration of leukocytes is extremely high). Either your own cells or a donor's cells are transplanted. Usually close relatives become donors.
- Additional therapy. Restores the condition of the blood, includes the introduction of blood elements.
Immunotherapy can also be used - a direction that uses immunological drugs.
Applicable:
- Medicines based on monoclonal antibodies,
- Adaptive cell therapy,
- Checkpoint inhibitors.
With a diagnosis such as acute myeloid leukemia, the duration of treatment is 6-8 months, but can be increased.
Clinical picture
Manifestations of acute myeloid leukemia are nonspecific - this means that at the initial stage the symptoms resemble those of other diseases.
Anemic syndrome
Due to insufficient hematopoiesis, the number of red blood cells decreases. General weakness, pallor, brittle nails and hair loss usually either do not attract the attention of the patient or his relatives, or are associated with other problems. As the disease progresses, weakness increases, shortness of breath appears even with minimal exertion, children stop playing outdoor games (in general, a decrease in a child’s activity is a reason to take a closer look at his health).
Hemorrhagic syndrome
Not only red blood cells, but also platelets become scarce in the blood. Blood clotting is impaired. Bleeding of varying intensity occurs: from pinpoint subcutaneous hemorrhages to heavy intracavitary hemorrhages (gastrointestinal, uterine, etc.).
Infectious and intoxication syndromes
Granulocytic leukocytes, belonging to the myelodine lineage, are cells whose function is to protect the body from microbes. They contain many proteins - natural antibiotics, peroxides, and other substances aimed at destroying the infectious agent. Inhibition of the hematopoietic germ also affects them, disrupting the body’s ability to fight pathogenic microbes. This is manifested by various purulent inflammations: skin abscesses, phlegmon, even sepsis. Any inflammation causes intoxication - poisoning by metabolic products of pathogenic microorganisms. Intoxication syndrome is manifested by such symptoms as:
- weakness;
- temperature increase;
- sweating;
- loss of appetite, weight loss;
- vague muscle pain.
Hyperplastic syndrome
Occurs in 30-50% of patients. Tumor cells fill not only the bone marrow, but also the lymph nodes, liver, and spleen. The organs enlarge, remaining painless, their consistency becomes doughy. Hyperplasia itself is not dangerous, but if lymph nodes that are located in a confined space (for example, the mediastinal cavity where the heart is located) grow, they can put pressure on vital organs.
Neuroleukemia
In 5-10% of children, leukemia cells create “metastases” - tumor growth sites in the cranial cavity, meninges, and large nerves. As a result, signs of damage to these organs arise: impaired sensitivity and function of the limbs due to infiltration of peripheral nerves, symptoms of meningitis and brain tumors due to the growth of infiltrate inside the cranial cavity.
Leukemia cells can form areas of extramedullary (literally translated - located outside the bone marrow) tumors in the bones, on the skin and mucous membranes, mammary glands, uterus and appendages, prostate, lungs. In this case, symptoms characteristic of the pathology of these organs arise.
Life forecast
The forecast depends on the following factors:
- AML type
- Sensitivity to chemotherapy
- Age, gender and health status of the patient,
- Leukocyte level
- The degree of involvement of the brain in the pathological process,
- Duration of remission,
- Indicators of genetic analysis.
If the disease is sensitive to chemotherapy, the leukocyte concentration is moderate, and neuroleukemia has not developed, the prognosis is positive.
With a favorable prognosis and the absence of complications, survival for 5 years is more than 70%, the relapse rate is less than 35%. If the patient's condition is complicated, then the survival rate is 15%, while the condition can recur in 78% of cases.
In order to detect AML in a timely manner, it is necessary to regularly undergo scheduled medical examinations and listen to the body: frequent bleeding, rapid fatigue, bruising from minor impacts, a prolonged causeless increase in temperature may indicate the development of leukemia.
Treatment of acute myeloid leukemia
Consists of accompanying therapy (CT) and antitumor chemotherapy (ACT). ST is universal for all types of acute leukemia. The absence of adequate ST excludes the achievement of the effect of PCT. There are induction and consolidation PCT, which should be carried out in specialized medical institutions. Induction therapy should include anthracyclines and cytosine arabinoside. Patients who do not respond to one or two cycles are considered refractory. When clinical and hematological remission is achieved, from one to several courses of consolidation therapy with cytosine arabinoside are carried out. For patients with an intermediate or poor prognosis in the absence of a related donor, unrelated allogeneic transplantation is indicated. The outcomes of therapy for acute leukemia can be: remission of the disease (duration of more than 5 years - recovery), early mortality (death during the first or second course of chemotherapy) or primary resistance (lack of remission after two courses of chemotherapy).
Essential drugs
There are contraindications. Specialist consultation is required.
- Daunorubicin (anthracycline antitumor antibiotic). Dosage regimen: IV, the dose of the drug is selected individually, taking into account the patient’s condition and the treatment regimen used.
- Cytarabine (antitumor, immunosuppressive drug). Dosage regimen: IV, at a dose of 100 mg/m2/day, two drop infusions of 3 hours each with an interval of 10 hours or continuously for 24 hours, per course - 500–1000 mg. SC, at a dose of 20 mg/m2 2–3 times a day. Course - 4–7 days (maximum up to 10 days).
Bone marrow transplantation
This procedure significantly increases the patient’s likelihood of recovery. The patient's relatives often act as donors. After conducting various compatibility tests, the patient begins to prepare for surgery for about one week. During this period of time, he undergoes radiation and chemotherapy.
During the operation, donor stem cells enter the patient's bloodstream, accumulate in the bone marrow and begin to function there within one month. During this period of time, the patient’s immunity is reduced, so he is prescribed medications to reduce the risk of rejection of donor cells. The doctor also prescribes antibacterial and antifungal medications. Gradually, the patient’s well-being improves, bones and soft tissues, blood are cleared of pathological cells and begin to function normally. Full recovery occurs after a few months, during which time the patient is under the supervision of the attending physician.
Note! Complete recovery is only possible with a stem cell transplant. In this case, they must be completely the same for the patient and the donor.
What is chronic myeloid leukemia?
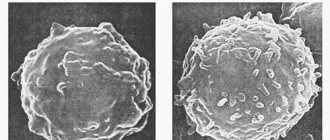
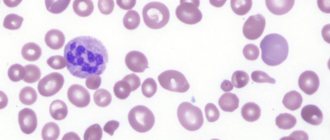
Blood smear of a patient with chronic myeloid leukemia
Chronic myeloid leukemia (CML) is a malignant neoplasm of hematopoietic tissue, accompanied by the progressive proliferation of immature granulocytes. The disease initially has a sluggish nature, gradually flowing into the stage of exacerbation with severe symptoms and the formation of systemic disorders. It is one of the most dangerous and disabling diseases.
CML is the first cancer in which a relationship between the development of carcinogenesis and a mutation in the gene has been identified. The characteristic anomaly is based on the translocation of chromosomes 9 and 22, that is, sections of these chromosomes change places, forming an aberrant chromosome. A mutated chromosome was identified by researchers from Philadelphia, so it was called the Philadelphia or Ph chromosome.
The study of the Ph chromosome and its influence made it possible to develop a new drug for suppressing oncological processes, thanks to which the life expectancy of patients has significantly increased. However, the disease still remains incurable. The number of primary CML is diagnosed in 1.5:100,000 of the population per year, the peak incidence occurs at the age of 30-50 years, 30% of CML is detected in people over 60 years of age, in children the disease is diagnosed in less than 5% of cases.
What is the essence of the problem?
In the picture you can see what the blood composition is in a healthy person, and how it changes with leukemia:
Many people are naturally concerned about the question: what is it? Acute myeloid leukemia (or acute myelocytic leukemia) is an oncological pathology affecting the blood system, when there is an uncontrolled proliferation of leukocytes of an altered shape. In addition, the blood test will also contain problems such as a decrease in the number of red blood cells, platelets and white blood cells from the normal category.
Blood diseases are particularly dangerous for humans. And this is not without reason, because it is the blood that is in close contact with all organs and systems in the body, it is the blood that carries vital hemoglobin and oxygen. Therefore, it is extremely important that blood circulation is fully and correctly established. The cellular composition should remain within normal limits.
Acute myeloid leukemia (AML) is a condition in which immature blood cells called blasts change. At the same time, the body experiences a lack of mature cells. The modified blasts increase virtually exponentially.
It is important to understand here that the process of cell change is irreversible and is not controlled by any medications. Blast cell leukemia is a serious and life-threatening disease.
Typically, all pathological processes in such a situation are localized in the bone marrow and peripheral circulatory system. Malignant cells actively suppress those that are not broken or spoiled and begin to infect literally everything in the body.
What is leukemia and can it be prevented? What is chemotherapy? Find out the answers to your questions by watching the following video:
Stages of disease development
Chronic myeloid leukemia has three stages of development:
- The chronic stage develops in the absence of timely treatment; the disease at this stage is diagnosed in 85% of patients. During this period, stability in the patient’s condition is observed, signs of pathology appear in minimal quantities and do not cause discomfort. The duration of this stage is three to four years, depending on how early treatment was started. CML is usually discovered incidentally during a blood test. If treatment is not started on time, the next stage of the disease occurs.
- The accelerated stage, during which the active growth of abnormal blood cells begins. This phase lasts about one year, and the development of new pathologies in addition to the abnormal chromosome is possible.
Note! The number of immature leukocytes at this stage is constantly increasing, but it is possible to return the disease to the chronic phase with proper treatment. Otherwise, the last stage of the disease develops.
- Blast crisis or end stage, which is the last phase of the disease, is characterized by the presence of new chromosome abnormalities. Here the bone marrow is completely replaced by pathological cells. This phase of the disease is similar to acute leukemia; if treatment is ineffective, the prognosis is unfavorable, and the disease ends in death. The blast crisis usually lasts about six months.
Some patients are already at the terminal stage of pathology when diagnosed, so the risk of death in this case is very high.
Reasons for the development of the problem
Leukemia, acute myeloid leukemia - all this is the same name for such a pathology. Naturally, many people are concerned about what leads to the development of such a problem. But, as is the case with other types of oncology, doctors cannot name the catalyst for changes in blood cells with 100% certainty. However, it is possible to identify predisposing factors.
Today, the main reason for the development of pathology is chromosomal abnormalities. Usually they mean the situation called the “Philadelphia chromosome”. This is a condition when, due to a disorder, entire sections of chromosomes begin to change places, forming a completely new structure of the DNA molecule. Then copies of such malignant cells are quickly formed, which leads to the spread of pathology.
According to doctors, this situation can be caused by:
- Exposure to radiation. For example, those at risk are those who are in production areas with a large amount of radiation, rescuers working at the site of removing rubble, as was the case at the Chernobyl nuclear power plant, patients who have previously undergone irradiation for the treatment of another type of oncology.
- Some viral diseases.
- Electromagnetic radiation.
- Impact of a number of drugs. Usually in this case they mean anti-cancer therapy due to its increased toxicity to the body.
- Heredity.
Those who are at risk should be screened regularly.
Pathogenesis
The disease develops due to a random chromosomal abnormality occurring in a stem cell. Normally, stem cells can develop into different types of cells in the body, including those that are elements of the blood. But when two chromosomes (9 and 22) are rearranged into the so-called Philadelphia chromosome, tyrosine kinase - an abnormal enzyme. It leads to increased production of white blood cells , which gradually multiply and fill the bone marrow. The cells then enter the peripheral blood, spleen and liver. In some cases, additional mutations develop that make myeloid leukemia resistant to treatment.
During the development of chronic myeloid leukemia, the main part of leukocytes is produced in the bone marrow. But some of them are also produced in the liver and spleen.
If in acute leukemia there are many blast cells in the body, then in the chronic form the number of leukocytes, which appear normal, increases significantly, and in some cases, platelets.
Gradually, a change in leukemia cells occurs, and the disease enters the acceleration phase, after which the blast crisis phase begins, when only immature leukemia cells are produced. Accordingly, the condition worsens, and the patient often has an enlarged spleen, fever, and weight loss.
Prognosis and prevention
If the chronic stage of the disease is diagnosed and a bone marrow transplant is performed in a timely manner, a complete recovery of the patient is possible. Most people die when they have an acceleration phase or blast crisis. In 10% of them, death occurs within two years of diagnosis. With the terminal stage of the disease, a person can live for another six months, but if the treatment gives positive results and remission begins, then life expectancy increases to one year.
Methods for the prevention of CML in modern medicine have not been developed, since the exact causes of the development of the pathology have not yet been clarified. Doctors recommend leading a healthy lifestyle, not abusing medications when treating various diseases, and also avoiding exposure to radiation.
( 2 ratings, average: 5.00 out of 5)
Treatment of blood oncology
At the initial stage of development of the disease, drug treatment is used. Doctors often prescribe A-interferon and Myelosan. Relief occurs in the sixth week of taking the drugs. Then maintenance therapy is carried out; in case of exacerbation of the disease, courses of treatment with Myelosan are carried out. If this drug is ineffective, use Myelobromol for three weeks. As a last resort, the doctor prescribes Dopan or Hexaphosphamide.
Also, to treat pathology, chemotherapy is used using chemicals that reduce the growth of tumor cells and promote their destruction. This method is used at different stages of the disease. It has side effects, which are expressed in disruption of the gastrointestinal tract, the appearance of allergic reactions, muscle pain, and cramps. After a course of chemotherapy, the doctor prescribes Interferon to restore the immune system.
If chemotherapy is ineffective, radiation therapy is used. It can also be used to prepare a patient for a bone marrow transplant.
Note! In some cases, the spleen is removed due to severe pain in the abdominal area, significant enlargement of the organ, or the threat of rupture.
In order to prevent the development of microscopic thrombosis and swelling of the retina, doctors prescribe leukocytophoresis. In this case, the blood is purified from pathological cells.