The development of medicine has stepped far forward over the past couple of decades. Along with conservative methods of examination, analysis and palpation, additional methods are used using special techniques and equipment. This is precisely what ultrasound refers to - the examination of internal organs using ultrasound.
Ultrasound has found widespread use in obstetrics and gynecology: a simple and relatively safe examination makes it possible to learn about the development of the fetus, its internal organs, the sex of the unborn child, gestational age, the structure of the placenta and note developmental disorders.
It is ultrasound waves that underlie Doppler ultrasound, which allows one to evaluate the structural features of blood vessels and the speed of blood flow in the placenta. Based on the data obtained, the observing doctor can notice the pathology in time or, conversely, exclude it, determine the risk of violations and take measures to eliminate them.
What is Doppler?
The procedure is performed on a conventional ultrasound machine equipped with special software. A regular ultrasound shows the condition and structure of the soft tissues of internal organs, deviations from the norm. Doppler ultrasound allows you to evaluate moving objects, such as the movement of blood through veins and arteries. It is the features of blood flow in the “mother-fetus” system that the gynecologist studies when receiving Doppler results.
Doppler ultrasound (Doppler), which is prescribed to almost all pregnant women, is based on the method of changing the frequency of the signal when reflected from moving particles.
The waves emitted by an ultrasonic sensor are reflected from moving particles much more often than from stationary particles. But blood moves through the vessels in different directions: the frequency of reflected waves from particles moving from the sensor increases, and towards the sensor decreases, which gives an idea of the speed of blood flow.
The result of changing the parameter is presented on the monitor screen, where the pattern of blood movement throughout the entire circulatory system of the fetus is shown in different colors (blue and red).
There is a widespread belief among women that ultrasound is quite harmful to the fetus, and with Doppler the intensity of the waves is even higher, so some expectant mothers simply refuse to undergo such an examination.
However, ultrasound has been performed in our country for almost two decades (quite a long time), which allows us to talk about its relative safety for the fetus. But other bloodless methods cannot obtain the amount of information that ultrasound gives us.
Prevention of BMD impairment during pregnancy
To ensure a healthy pregnancy, gynecologists recommend that expectant mothers:
- maintain a good mood, avoid emotional shocks, as well as heavy physical work;
- put an end to bad habits once and for all;
- eat tasty and healthy foods;
- regularly ventilate all areas of your home, walk outside every day;
- master gymnastics for pregnant women, if desired, combine it with yoga exercises;
- monitor your weight;
- Do not miss scheduled examinations with a gynecologist.
High-quality diagnostics and the great capabilities of modern medicine make it possible to identify and treat various pathologies at the earliest stages of development. However, a woman’s desire to have healthy offspring is also of great importance: in order for pregnancy to proceed smoothly, the expectant mother must carefully monitor her health before pregnancy and approach planning the baby wisely.
How is Doppler sonography performed?
This study is carried out in a supine position, the skin of the expectant mother’s abdomen is treated with a special gel-like product that transmits ultrasonic waves, and the ultrasound specialist moves the sensor over the abdomen, receiving the results on the monitor.
Basically, no preparatory measures are required from the expectant mother. The only thing they may be asked to do before the study is to limit food intake a couple of hours before the procedure.
What does a Doppler ultrasound show:
- The work of the fetal heart muscle at rest and in motion;
- Condition of the valves and blood vessels of the child’s heart;
- The work of the peripheral circulatory system;
- Blood circulation in the umbilical cord and placenta;
- Functioning of the pregnant woman’s organs: kidneys, heart, circulatory system.
Varieties of the method
There are duplex
dopplerography and
triplex
. The first option results in a monochrome two-dimensional image, from which you can obtain data on the movement of blood through the vessels and programmatically calculate its speed.
But the most informative is triplex Dopplerography (color mapping), which gives an idea not only of the speed of blood movement, but also of the direction, as well as the anatomical state of the vessels. On the monitor, the doctor sees lines painted in two primary colors - red and blue, indicating the movement of blood in the direction from the sensor and towards it.
Signs of BMD impairment during pregnancy
If the body independently compensates for imperfect blood flow, the woman will not feel anything bad, and deviations will be discovered only as a result of a thorough examination.
In acute circulatory disorders, as well as chronic decompensation, obvious signs of the disorder appear:
- fetal movements suddenly become more active or disappear completely (we remind you that at week 28 the baby’s normal movements are 10 episodes per day). If such “strangeness” is detected, you need to consult a doctor right away;
- too slow growth of the abdomen in circumference. It is detected provided that the expectant mother responsibly attends all scheduled examinations in the residential complex. This symptom occurs due to a deficiency of amniotic fluid;
- gestosis;
- high blood pressure;
- excessive weight gain;
- severe swelling in the lower legs;
- the presence of protein in the urine;
- vaginal bleeding. This is the most dangerous sign indicating premature detachment of the child's place. The expectant mother needs immediate hospitalization.
Indications for the study
Dopplerography has made it possible for doctors to determine whether the baby is developing normally in the womb, what disturbances exist in the functioning of the “mother-placenta-fetus” system, to monitor all deviations in real time, to monitor the functioning of certain vessels during pregnancy and more.
The use of Doppler ultrasound during pregnancy allows
- Observe the movement of blood during contractions of the fetal and maternal cardiac muscles
- Judge the size, number and location of blood vessels
- Determine the exact location of pathology occurrence
Doppler testing is recommended for all pregnant women between 30 and 34 weeks, regardless of the presence of certain pathologies.
Today there is hardly a single pregnancy that proceeds without complications or any disturbances. Therefore, even if no deviations are found in the test results of the expectant mother, the observing gynecologist is obliged to refer her for this examination.
The third trimester was not chosen by chance: it is at this time that the placenta and fetus are already sufficiently developed to see all the deviations that are possible. But the birth is still far away and doctors still have the opportunity to correct certain deviations.
However, there are a number of indications for unscheduled Doppler measurements at 20-24 weeks. Such indications may include alleged and actual violations:
- Suspected fetal hypoxia
- Deviations in fetal development: congenital defects noticeable with conventional ultrasound
- Uneven development of one of the fetuses during multiple pregnancy
- Low/high hydramnios
- Premature aging of the placenta
- Inconsistency between the size of the fetus and the due date
- Chronic diseases in a pregnant woman: diabetes mellitus, hypertension, kidney disease, gestosis, vasculitis
- Rhesus conflict between mother and child
- Wrapping the umbilical cord around a baby's neck
- Incorrect position of the fetus in the womb
- Noticeable abnormalities in cardiotocography (CTG)
The doctor may also refer the expectant mother for an unscheduled examination in case of early/late pregnancy, abdominal trauma, unfavorable outcomes of previous pregnancies, or delayed birth.
loading…
Mechanism of BMD disturbance during pregnancy
If the blood flow supplying the placenta is disrupted, placental insufficiency develops. This trouble can overtake a woman at any stage of pregnancy. The pathological condition occurs in two forms:
- acute - develops spontaneously regardless of gestational age. It may even appear at the time of birth. The child is exposed to acute oxygen starvation, which can cause death. This also increases the risk of premature placental abruption;
- chronic - diagnosed mainly after the 13th week of pregnancy, and pronounced symptoms of the pathological condition appear already in the later stages of pregnancy. The main reason for the development of this form of placental insufficiency is considered to be premature aging of the child's place due to excessive accumulation of fibrin on the villi.
Both acute and chronic placental insufficiency, depending on the severity of the disorder, can provoke intrauterine death of the child.
Dopplerometry norms and deviations: tables
As with any other study, Doppler ultrasound distinguishes between normal values and deviations. But, since all pregnant women are different, even with a favorable course of pregnancy there cannot be the same values. Therefore, a certain range is allowed. With Doppler ultrasound, the doctor receives the following indicators:
Indicators of the norm of the uterine artery resistance index
is an indicator used to assess blood flow in the large vessels of the uterus.
Standard indicators of the pulsatility index of the uterine arteries
Two uterine arteries are examined - left and right, and their indicators may vary. This is not a deviation, the main thing is that the values do not go beyond the acceptable range.
If there are deviations in one indicator, uteroplacental circulation can be assumed. If deviations in both indicators are recorded, this may indicate a violation of the uteroplacental blood flow.
Abnormalities in the indicators of the uterine arteries are allowed only at 18-21 weeks of pregnancy, which may indicate an incomplete adaptive physiological process of cytotrophoblast invasion. Usually the doctor prescribes repeat Doppler testing of the fetus after a couple of weeks.
Standard indicators of the systole-diastolic ratio in the fallopian tubes
Standard values of the umbilical cord artery resistance index
Standard values of the pulsatility index of the umbilical cord arteries
Indicators of diastolic blood flow values may be zero or reverse, which indicates a critical condition of the fetus, the death of which will occur in 2-3 days. If the gestational age exceeds 28 weeks, then an emergency caesarean section is prescribed to save the baby's life.
Standard values of the systole-diastolic ratio of the umbilical arteries
Deviations in the values of blood flow in the umbilical cord lead to delayed development of the child.
Doppler ultrasound norms: middle cerebral artery of the fetus
Peak velocity in the fetal middle cerebral artery
Standard values of the systole-diastolic ratio in the middle cerebral artery
Standard values of the pulsatility index of the fetal aorta
Normative values of the fetal aortic resistance index
Standard values for fetal aortic systolic velocity
Standard values of the systolic-diastolic ratio of the fetal aorta
Blood flow disturbances in the fetal aorta can only be seen after 22-24 weeks of pregnancy.
The value of measuring the hepatic artery resistance index in the diagnosis of liver cirrhosis
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Introduction
Liver cirrhosis is caused by chronic necroinflammatory liver disease leading to fibrosis and nodular regeneration. The clinical consequences of cirrhosis develop as a result of a combination of impaired liver cell function, obstruction of bile flow and changes in hepatic blood flow with disruption of normal liver structure [1]. In liver cirrhosis, the increased amount of connective tissue leads to higher resistance not only to blood flow in the portal vein, but also in the hepatic artery [2]. Not every case of liver cirrhosis exhibits its typical sonomorphological signs, such as narrow hepatic veins, regeneration nodules and an uneven surface [3]. The introduction of color and duplex Doppler studies makes the identification of the hepatic artery and its hemodynamics an accessible non-invasive study for the diagnosis and monitoring of liver cirrhosis and portal hypertension [4]. The total volume of hepatic blood flow is approximately 1.5 liters per minute. The portal veins supply approximately 75% of the blood, while the hepatic arteries supply only 25%. The development of cirrhosis affects hemodynamics [5]. Calculation of the hepatic artery resistance index can provide an indirect characteristic of blood flow in the hepatic artery and direct information about hemodynamic changes in the vascular bed of the hepatic parenchyma [4].
Materials and methods
We studied 100 patients admitted to the Department of Liver and Biliary Pathology of the Faculty of Medicine of the University of Alexandria. Biopsy-proven cirrhosis was diagnosed in 55 patients. Diagnosis of cirrhosis using a combined clinical examination, laboratory methods and ultrasound data was carried out in 36 patients. In the latter, it was impossible to perform a liver biopsy due to an increase in prothrombin time or the patients’ refusal to do this procedure. Nine patients were excluded from the analysis of the results because a clear waveform of blood flow in the hepatic artery could not be obtained.
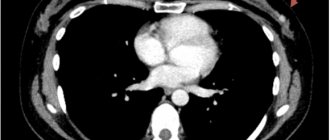
First, the hepatic artery was located using color flow mapping, then pulsed Doppler was used to clearly assess the waveform of the blood flow. The interrogating volume was placed into the lumen of the hepatic artery just before its bifurcation into the main right and left branches.
The resistance index (RI) was calculated using the maximum systolic velocity A and maximum diastolic velocity B as follows [6]:
IR = (A - B)/A.
The diameter of the hepatic artery was also measured. As a control group, 20 volunteers with normal liver function and normal liver ultrasound findings were examined. A clear waveform of hepatic blood flow was obtained in only 17 people from this group.
results
In the group of patients with liver cirrhosis, including 73 men and 27 women, the average age was 49.6 years; the youngest was 28 years old and the oldest was 64 years old. The average age of the control group, which included 14 men and 6 women, was 45.3 years. In the groups of patients and healthy people there were no differences in the hepatic artery resistance index by age and gender. The resistance index in the control group was 0.62, while the average value of the resistance index in the cirrhosis group was significantly higher - 0.76 (p < 0.0001). In patients with established cirrhosis, there was no significant increase in the resistance index compared to patients with early stage cirrhosis. Portal vein thrombosis was diagnosed in 11 patients and reverse flow in 5; The average resistance index in these two groups was 0.80, with no significant differences between the first and second, but it was significantly higher than in the group of patients with cirrhosis without portal vein thrombosis or reverse blood flow.
Using a cutoff rate greater than 0.70, the resistance index had a sensitivity of 66, a specificity of 67, and an accuracy of 68%. The average diameter of the hepatic artery in the control group was 2.5 mm, while in patients with cirrhosis it exceeded 4.5 mm, i.e. There was a significant dilatation of the hepatic artery (p<0.001).
Discussion
Ultrasound signs of liver cirrhosis are: changes in the hepatic echostructure, the presence of nodes, enlargement of the caudate and reduction of the right lobe of the liver, as well as the presence of indirect signs such as portal hypertension, splenomegaly, the appearance of collaterals and ascites. Detection of hemodynamic changes in the hepatic vascular bed in cirrhosis may be another sensitive sign that helps in the diagnosis and prognosis of cirrhosis. Devices with the capability of highly sensitive color Doppler examination allow mapping of the hepatic artery along its entire course. In patients with cirrhosis, its diameter increases, which facilitates locating. In the present study, the average diameter of the hepatic artery of patients with cirrhosis exceeded 4.5 mm, while in the control group it was only 2.5 mm. Color Doppler examination primarily helps in the diagnosis of dilatation of the hepatic artery and its differentiation from the dilated common bile duct.
Rice. 1.
A group of dilated convoluted capillaries, like channels, at the porta hepatis, representing a large cavernous transformation of the portal vein.
Rice. 2.
Complete thrombosis of the portal vein with an echogenic “old” thrombus in its distal two-thirds and a “recent” thrombus of lower echogenicity in its proximal third.
It appears that the hepatic artery dilates to increase blood flow into the hepatic parenchyma and to compensate for the decrease in portal blood flow. Vassiliades et al. (1993) showed that the diameter of the hepatic artery in patients with cirrhosis is 0.64 ± 0.06 mm. Leen et al. (1993) demonstrated an increase in blood flow through the hepatic artery in patients with cirrhosis, indicating a redistribution of blood flow between the portal vein and the hepatic artery. Moreover, the dilated hepatic artery may be the starting point for the development of portal vein thrombosis or reverse portal blood flow. The resistance index was chosen due to its independence from errors arising from incorrect selection of the Doppler scanning angle, which is especially important for the hepatic artery, which usually has a tortuous course, and selecting the angle of the sensor parallel to its lumen is not an easy task.
Rice. 3.
Partially reversed blood flow in the portal vein during exhalation is called “partial hepatofugal flow.”
Rice. 4.
Variants of the image with different courses of the normal hepatic artery.
Visualizing the hepatic artery and obtaining a clear Doppler recording of blood flow in it takes time. In addition to known normal anatomical variations, the presence of ascites, gas in the abdominal cavity, lack of cooperation with the patient (who cannot hold his breath for a sufficient period of time), and obesity may be obstacles to the examination of the hepatic artery. In the present study, the resistance index could not be calculated in 9 patients and 3 members of the control group due to the difficulty of obtaining a clear Doppler spectrum or even the impossibility of locating a normal hepatic artery, especially in healthy individuals.
Rice. 5.
Normal blood flow waveform with normal IR=0.6.
In the present study, there was no significant correlation between the severity of cirrhosis and the hepatic artery resistance index, which was previously shown by Vassiliades et al. (1993). However, there is a significant increase in the hepatic artery resistance index if cirrhosis is accompanied by portal vein thrombosis or reverse flow. In a study of hepatic artery resistance in cirrhosis with and without portal vein thrombosis, Saccrdoti et al. showed that the resistance index in cirrhosis without portal vein thrombosis is 0.71 ± 0.07, while in patients with cirrhosis with portal vein thrombosis it is 0.81 ± 0.06.
Rice. 6.
The trunk of the celiac artery and its Y-shaped bifurcation into the hepatic and splenic arteries.
It appears that the pathophysiological mechanisms of increased hepatic artery resistance develop in parallel with the increase in portal resistance. The hepatic artery dilates to compensate for the increased resistance from its hepatic bed, which ultimately leads to increased blood flow, whereas in patients with liver neoplasms, particularly metastases, the hepatic artery dilates with increased blood flow to accommodate the increased blood supply required for low-resistance vascular bed of neoplasms. These data were clearly presented in the study by Leen et al. (1993) when studying changes in hepatic perfusion in patients with liver metastases in comparison with patients with cirrhosis.
Rice. 7.
Curved trunk of the celiac artery and curved hepatic artery.
The diameter of the hepatic artery increases in parallel with the increase in the average blood flow velocity in it, while the diameter of the portal vein increases as the average blood flow velocity in it decreases. Thus, a redistribution of hepatic perfusion occurs between the hepatic artery and the portal vein. In 1995, Joynt et al. published a study that showed a marked increase in hepatic artery resistance index in healthy people after eating, which was not observed in patients with severe liver disease. This may be because the resistance index is already increased in patients with cirrhosis, but Joynt et al. did not reveal changes in the diameter of the hepatic artery after eating.
Rice. 8.
The hepatic artery is dilated to 6 mm with a parallel course in relation to the portal vein. Increased blood flow through the hepatic artery with superimposed spectra of maximum systolic velocity. IR=0.71.
It should be emphasized that the use of color Doppler and pulsed Doppler to measure hepatic artery resistance index is a reliable, relatively simple and sensitive non-invasive method that increases the possibility of diagnosing cirrhosis. A dilated hepatic artery may be an initial clue to the diagnosis of portal vein thrombosis or flow reversal when there is also a significant increase in the hepatic artery resistance index. The resistance index identifies and explains the redistribution of blood flow between the portal vein and the hepatic artery in liver cirrhosis.
Literature
- Herlong H, Andrew S. Cirrhosis. In: Pitt. HA, Feirucci J, eds. Hepatobiliary and pancreatic disease. Boston: Little, Brown and Company 1995: 3-30.
- Becker D, Gunter E, Seutter F. The hepatic artery resistance index: Distinction of cirrhotic livers from non-cirrhotic livers. Abstract. The American Association for the Study of Liver Diseases. Gastroenterology 1995; 108: 1021-71.
- Ralls P.W. Color Doppler sonography of the hepatic artery and portal venous system. A/R1995:155:517-25.
- Goncalvesova E, Kovac A. Color Doppler sonography in the diagnosis of portal hypertension in patients with liver cirrhosis. Abstract: The 2nd World Congress of International Hepatopancreaticobiliary Association, Bologna, Italy, 1996.
- Cioni G, Tincani E, Cristani A. Does the measurement of portal flow velocity have any value in the identification of patients with cirrhosis at risk of digestive bleeding? Liver 1996; 16: 84-87.
- Piscalgia F, Zironi G, Siringo S. US Doppler investigation of hepatic artery hemodynamics in liver cirrhosis and chronic active hepatitis. Abstract. The 30th Annual Meeting of the European Association for the Study of the Liver, Copenhagen, Denmark, 1995.
- Vassiliades VG, Ostrow TD, Chezmar JL, Hertzler GL, Nelson RC. Hepatic arterial resistive indicators: correlation with the severity of cirrhosis. Abdom Imaging 1993; 18: 61-65.
- Saccrdoti D, Merkel C, Bolagluesi M, Amodio P, Augeli P, Gatta A. Hepatic arterial resistance in cirrhosis with and without portal vein thrombosis: Relationships with portal hemodynamics. Gastroenterology 2995:108:1152–1158.
- Bolandi L, Libassi S, Gaiani S, Zironi G, Benzi G, Sauti V, Barbara L. Liver cirrhosis: changes in Doppler Waveform of Hepatic Veins. RAD 1991;178:513-516.
- Leen E, Goldberg [A, Anderson JR, Robertson J, Moule B, Cooke TG, Me Ardle CS. Hepatic perfusion changes in patients with liver metastasis: Comparison with those patients with cirrhosis.Gut 1993;34:554-557.
- Joynt LK, Plott JP, Rubin JM, Ellis JH, Bude RO. Hepatic artery resistance before and after standard meal in subjects with diseased and healthy livers. RAD 1995;196:489-492.
- Pierce MF, Swwell R. Identification of hepatic cirrhosis by duplex Doppler ultrasound value of the hepatic artery resistive index. Australs Radiol 1990;34:331-333.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
How to understand if there is hypoxia
It is based on the results of a Doppler ultrasound that the gynecologist can see whether oxygen starvation of the fetus is occurring, whether the child is receiving all the necessary substances and what to prepare for during childbirth.
What abnormalities can fetal Doppler ultrasound detect?
- Exceeding the values of IR and SDO in the uterine arteries is a sign of oxygen starvation of the fetus. This can subsequently lead to delayed growth and development.
- Feto-placental insufficiency will be indicated by an excess of Doppler values for the umbilical cord artery. This is a vascular pathology that leads to fetal suffering. This is also a sign of gestosis.
- Hypoxia of one of the fetuses during multiple pregnancy (transfusion syndrome) is indicated by the difference between the IR and SDO indicators in the umbilical cords.
- The child may feel unwell if labor is delayed, diabetes mellitus in the pregnant woman, or Rh conflict. This is indicated by an increase in SDO and IR in the aorta.
- But a decrease in these same values in the carotid and cerebral arteries is observed in extremely severe conditions of the fetus, since in this case only the main organs that support life are supplied with blood and oxygen. In such cases, it is recommended to immediately carry out artificial labor.
Dopplerography of the fetus is one of the important diagnostic measures carried out by a pregnant woman, revealing disorders in the blood vessels and the utero-placental-fetal system. Thanks to the results of the blood circulation analysis, the doctor makes a decision on the tactics of managing pregnancy and childbirth in the future.
Types of BMD disorders during pregnancy
Placental insufficiency is divided into 4 types, which are distinguished by the strength of the pathological effect on the fetus and the ability of the mother’s body to prevent this harmful effect:
- compensation - the mother’s body makes up for the lack of MPD, activating blood flow through other pathways, so the fetus is not threatened by hypoxia and it continues to grow in accordance with the norms. The child is born on time and fully develops;
- subcompensation - the female body is unable to compensate for the deficiency of oxygen and nutrients to the fetus, so the child lags behind in development and risks getting one or more of the numerous congenital defects;
- decompensation - all adaptation mechanisms are completely destroyed, so there is no chance for the normal development of pregnancy. In most cases, intrauterine death of the fetus occurs, since the small organism is overcome by defects incompatible with life;
- critical - completely untreatable. Changes in the placenta are irreversible, so the fetus is obviously doomed.
Is this diagnostic method dangerous?
The absolute safety of Doppler ultrasound (as well as conventional ultrasound) has long been proven by specialists.
Firstly, ultrasound cannot harm either the mother or the child.
Secondly, ultrasound examination is not fraught with any consequences for the human body.
Thirdly, the abdominal method eliminates possible injuries, as it is as painless and accurate as possible.
Fourthly, Doppler testing itself is possible thanks to a technological breakthrough and depends on the capabilities of the equipment in the diagnostic room, and not on any special manipulations of the doctor, therefore it is also safe.