Hello everybody! Laparoscopy in gynecology is used very widely. This is understandable - minimal risks, less pain, shorter rehabilitation times in comparison with classical methods of surgical gynecology. When medical conditions require removal of the uterus, laparoscopy is often the surgical method of choice. Today we'll figure out why.
Indications for hysterectomy
In surgical gynecology, the procedure for amputation of the uterus has its own name - hysterectomy; it is indicated in situations where medical therapy has not had a positive result or when the patient sought help too late.
In some European countries, hysterectomy is performed even on those patients who have a hereditary tendency to develop uterine cancer or according to the wishes of a woman who does not want to have her own children and is afraid of developing complex gynecological pathologies.
For representatives of the fairer sex of our country, the reproductive function is very significant, so it is very rare to meet a patient who, without a doctor’s recommendation, would have the reproductive organ removed.
Hysterectomy may be indicated by a doctor for such disorders or diseases of the reproductive and genitourinary areas as:
- Malignant neoplasms in the uterine cavity and its tubes;
- Myoma in the uterine cavity;
- Excessive growth of the endometrium;
- Adenomyosis;
- Fibroids during menopause;
- Prolapse, prolapse of the reproductive organ;
- Numerous or single formations on the uterus;
- Dying of fibromatous nodes;
- When gender change;
- Mechanical disruption of the integrity of the uterine body.
Excision of the uterus is prescribed by oncologists only in extreme cases, because its implementation completely deprives a woman of reproductive quality. This measure is carried out for fibroids and other complex pathologies.
Myoma
Intervention to remove fibroids in the uterine cavity is carried out in cases of significant growth of miasmatic tumors, large volumes of tumors and other complex conditions, if it is not possible to perform myomectomy or embolization.
Excision of the uterus for fibroids - the result may not always please the patient, since during the operation sometimes not only the uterus is removed, but also its appendages, fallopian tubes, and in 40% of situations the ovaries are also excised.
The term fibroid in medical practice refers to a benign neoplasm of a muscle and connective structure.
Often the formation develops in the uterus. Fibroids come in all sizes.
When the myomatous nodes of the tumor are more than 6 cm and the uterus is of significant size, similar to the 12th week of gestation, then such a benign neoplasm is large.
In order to get rid of fibroids, one of the types of intervention may be indicated: laparoscopic or abdominal myomectomy, intervention to excise the reproductive organ.
Hysterectomy for this pathology is indicated as a last resort, when other methods have failed, or the patient’s age category is over 40 years.
Endometriosis
The process of growth of the mucous layer of the uterine body into the ovaries, peritoneum, fallopian tubes and other areas in which it should not be present is called endometriosis in medicine.
This pathology is associated with inflammation of nearby organs, on which the internal uterine layer grows, painful manifestations during critical days, and vaginal discharge.
In some cases, with endometriosis, it becomes necessary to perform uterine excision.
However, this measure is not always effective in completely eliminating the disease.
Hysterectomy of the uterus for this pathology is indicated for patients who do not want to have more children.
Cervical cancer
In order to eliminate the threat to the patient’s life, specialists may prescribe a hysterectomy for cervical cancer.
In such a situation, radical intervention is often carried out.
The cervix, upper fragment of the vagina, uterus, fallopian tubes, ovaries and nearby tissues, and lymph nodes are excised.
After a hysterectomy and excision of a malignant neoplasm, the patient is prescribed a course of radiation treatment and radiotherapy.
By the time the operation is performed, it can predetermine the further formation of malignant growth in the body.
Necrosis of fibromatous nodes
The most severe deviation of uterine fibroids, associated with a lack or absence of life-sustaining nutrition of fibromatous cells with the prospect of developing painful sensations and swelling. Palpation of the affected area increases pain, provokes vomiting, fever and irritation of the peritoneum.
Penetration of infection causes more significant manifestations of pain. The type of operational measure is determined purely individually. The result of the operation is related to the age category of the patient and her general state of health.
Prolapse and prolapse of the uterus
Providing factors for this deviation are considered to be weakness of the muscles in the pelvis and peritoneum. The formation of the disease is helped by inflammation, endocrine disorders, numerous births and physically hard work.
If there is no expected result from treatment at the initial stage of the disease, a radical method becomes necessary - hysterectomy. excision implies two ways of developing events:
- Uterine and vaginal removal;
- Fragmental excision of the vagina, allowing sexual activity.
Indications
Laparoscopic hysterectomy can be used for:
- combination of cervical diseases (scars, hypertrophy, ectropion, precancerous changes) with multiple fibroids;
- recurrent or atypical endometrial hyperplasia in women over 40 years of age;
- adenomyosis;
- uterine cancer, multiple or atypical polyps;
- An emergency operation is performed after childbirth, when the placenta accreta does not detach or the myometrium cannot contract.
Removal of the uterus and ovaries by laparoscopy is used for progressive ovarian tumors, a combination of sclerocystic disease or apoplexy of the ovaries with a tumor of the uterus, purulent inflammation of the ovary, when the uterine tissue and neighboring organs are involved in the purulent melting.
The operation is performed laparoscopically through small (usually 0.5-1.5 cm) holes
In women over 50 years of age, hysterosalpingo-oophorectomy is performed when there is heavy uterine bleeding or tumor growth in one of the reproductive organs. Hysterectomy and removal of one or two appendages are performed for patients in the older age group who are at risk for developing a malignant tumor.
“Removal of the uterus” refers to the varying scope of the operation, which depends on the disease:
- Supravaginal amputation. This is the name for removing the body of the uterus, when its cervix and appendages remain in place. It is performed for large-volume fibroids, adenomyosis, postoperative complications and an atypical form of endometrial hyperplasia, heavy uterine bleeding and pelvic pain, when the cause of these phenomena is not clear.
- Total hysterectomy. In this case, both the body and the cervix are removed, but the tubes and ovaries remain in place. This intervention is performed for endometrial cancer.
- Radical hysterectomy. This is called removal of the uterus and appendages. The method is applicable only if a cancerous tumor is detected that spreads to one of the appendages. If the cancer spreads from the body to the cervix, the initiated laparoscopic intervention is expanded to laparotomy. Not only the uterus, its cervix, tubes and ovaries are removed, but also the inguinal and pelvic lymph nodes, and often the upper parts of the vagina.
The older the woman, the more doctors are inclined to perform more radical surgery. Gynecologists in the USA even perform removal of the uterus along with the cervix in women over 40 years of age who do not have diseases of the reproductive system. Thus, they say, the risk of developing high-grade ovarian cancer is reduced by more than 3.5 times. This is especially important for those who are hereditarily predisposed to the development of cancer, including breast cancer.
Is surgery really necessary?
The advisability of performing a surgical intervention aimed at excision of the uterine appendages and the uterus itself is determined exclusively by the doctor
Preparing for surgery
To be fully prepared for surgery, the surgeon must stock up at least 0.5 liters of blood, which, if necessary, can be transfused to the patient.
If the patient has second or third degree iron deficiency, then before the intervention she receives a blood transfusion.
If atrophic colpitis is diagnosed, the patient undergoes a course of therapy aimed at normalizing the damaged tissues.
Those with a known tendency to form blood clots are prepared with special attention.
Such patients use drugs to reduce the development of blood clots, regulate blood density, and bring arteries and blood vessels to normal tone.
If a tendency to varicose veins is noticed, the patient should undergo an ultrasound examination of the legs. To avoid infection during surgery, antibiotics are prescribed and administered to the patient under anesthesia.
In practice, there is an inapplicable rule in surgery: before any even the slightest significant surgical procedure is performed, each patient must certainly receive advice from specialists such as a phlebologist and a vascular surgeon.
Analyzes
Since the operation of excision of the uterus and ovaries is quite difficult, after its implementation many complications appear, therefore, the person being operated on must undergo tests to determine the condition of other organs, blood and the rest:
A vaginal smear is required to determine the presence of mutating cells.
- Testing for sexually transmitted infectious diseases is carried out.
- The Rh factor of the patient is detected.
- Blood and urine tests are performed.
- Testing for blood anticoagulation (clotting) is likely using the Lee White method.
- Testing for infectious diseases is very important.
- If cancer is suspected - MRI, ECG.
- Examination of the lungs using radiography.
- Ultrasound of the pelvic organs.
Bowel preparation
The following activities need to be completed and prepared:
- Carrying out a 3-day diet that excludes the consumption of toxins and fiber;
- Exclude legumes, bakery and vegetable, berry, and fruit products;
- Do not eat food the night before surgery (be patient for at least 8 hours before surgery);
- Do not eat or drink directly on the day of surgery in order to prevent vomiting from the effects of anesthesia;
- Empty the stomach immediately before the hysterectomy using an enema.
Moral preparation
Removal of the main reproductive organ from the female body is a powerful stress, in particular for young women. The surgeon needs to explain why the intervention is necessary and how it will be carried out.
And the patient’s concerns about a sexually active life after a hysterectomy are unfounded, because the elimination of some organs of reproductive function does not affect the degree of libido.
Progress of the operation
In gynecological practice, for the most part, the method of laparoscopic or assisted vaginal subtotal or total removal of the uterus is used, leaving appendages on at least one side (when possible), which, without taking into account other advantages, helps to reduce the degree of manifestation of post-hysterectomy sensations.
The operation with a combined access consists of 3 stages - two laparoscopic and vaginal.
The initial stage consists of:
- introduction into the abdominal space (following the introduction of gas into it) through mini-incisions of manipulators and a laparoscope, which contains a lighting system and a video camera;
- implementation of laparoscopic diagnosis;
- release of present adhesions and identification of ureters when required;
- the use of binding linen or silk threads and crossing the round ligaments of the uterus;
- mobilization (separation) of the bladder;
- the use of binding linen or silk threads and crossing the uterine tubes and one’s own uterine ligaments or excision of the ovaries and uterine tubes.
The next stage is presented in:
- dissection of the outer vaginal wall;
- passing through the vesicouterine ligament, following the retraction of the bladder;
- making an incision in the mucous membrane of the deep vaginal wall and applying sutures to stop bleeding on it and on the peritoneum;
- applying binding linen or silk threads to the uterosacral and cardinal ligaments, as well as to the uterine veins to intersect these tissues;
- pulling the uterus closer to the wound and cutting it off or dividing it into parts (if it is significant) and removing them one by one.
- Applying stitches to the stumps and to the vaginal mucosa.
At the third stage , laparoscopic monitoring is carried out again, during which minor bleeding capillaries (if any) are ligated and the pelvic space is drained.
Pre-operative examination
Before the question of prescribing a hysterectomy arises, the attending physician will determine its necessity based on tests, the condition, and the availability of adequate alternative treatments.
To clarify the localization of pathological foci and study their prevalence, examinations should be carried out with a high degree of information content.
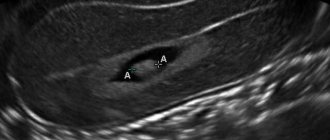
Endovaginal and abdominal sonogram (ultrasound)
Intravaginal and abdominal ultrasound examinations will help confirm the presence and determine the location of adenomyosis or fibroids, and also show the condition of the ovaries.
MRI using contrast
MRI will provide high-quality images that will clarify the suspected diagnosis of endometriosis, adenomyosis, and fibroids. This test allows the surgeon to visualize the ureters, which carry urine from the kidneys to the bladder.
Diagnostic curettage of the uterine cavity during hysteroscopy
In the operating room, the operating gynecologist examines the uterus using hysteroscopic equipment to exclude:
- cervical cancer or uterine cancer,
- diffuse adenomyosis,
- fibroids of the submucosal layer,
- or any other signs requiring a hysterectomy.
Then, the contents of the cervix and then the endometrium are scraped separately. Biological materials taken as a result of curettage are sent for histological examination to clarify the cellular composition, detect atypical cells, and the degree of their foreignness.
Based on the results of the studies, the time of the operation is assigned, its volume, and the method of intervention are determined.
Preparation for laparoscopy is no different from how patients are prepared for other surgical interventions.
- Before the operation you will be referred to a general practitioner to ensure that there are no contraindications that could cause problems during the operation;
- If the therapist identifies conditions that require drug correction, for example, uncontrolled hyperglycemia, arterial hypertension, cardiac arrhythmia, then you will be prescribed medications that improve the condition before surgery. This will eliminate unwanted consequences afterwards;
- Before the operation, you will donate blood, urine, and, if necessary, smears from the vagina and cervix; You will undergo an electrocardiographic examination and a chest x-ray;
- Immediately before the operation - one day before, the anesthesiologist will consult you to choose the type of anesthesia, to determine the presence or absence of contraindications to certain medications;
- Do not eat anything the evening before the operation;
Types of hysterectomy
Excision of the uterus is not only the removal of the affected organ, since hysterectomy is often associated with surgery on other anatomical tumors.
Depending on the volume of intervention performed, hysterectomy is divided into:
- subtotal – removal of the uterus (the cervix remains)
- total - surgery to excise the cervix and the uterus itself (extirpation) - surgery of the uterus and ovaries with appendages, radical cervix - removal of the organ with appendages, the upper part of the vagina, the tissue that grows around the uterus and regional lymph nodes.
According to the method by which access is provided, the following types of removal of the reproductive organ are distinguished:
- laparotomy hysterectomy (the uterus is removed through a longitudinal or transverse section of the abdominal wall)
- removal of the organ laparoscopically (a small number of punctures, from 2 to 4, in the abdominal wall, through which the laparoscope and devices are introduced)
- Vaginal hysterectomy – access to the diseased organ is performed through the vaginal cavity.
Radical hysterectomy is performed in the case of a malignant neoplasm of the uterus involving the cervix in the pathological process or in the case of a malignant tumor of the cervix.
Total removal is required for large uterine fibroids, growing endometriosis, associated diseases (formations) of the uterus and cervix, and in addition for women over 45.
In other situations, the main reproductive organ is amputated.
Whether appendages must be removed or not - this issue is often decided at the time of resection, when the organs can be seen. The method by which admission will be made largely depends on the operating surgeon. But in some situations, a woman can be given the right to choose.
The advantages of abdominal removal include affordable prices, confidence, a reduced risk of intraoperative complications, and the possibility of it being carried out in almost every women's department. The disadvantages include: a significant scar on the abdomen, a long stay in the hospital (10 days), a long recovery period (4 - 6 weeks).
The advantages of laparoscopic hysterectomy include: discharge after 5 days, a short recovery period (2 - 4 weeks), no visual effect (no scars), a reduced risk of adhesions in the abdomen, and as a result a reduced likelihood of adhesions with a pronounced painful syndrome.
The disadvantages include: a very expensive operation, the prospect of switching to laparotomy, is carried out exclusively in large cities (medical centers and institutes).
Vaginal hysterectomy is easily tolerated, there are no scars on the abdomen, the recovery period is shorter, 3 - 4 weeks, there is almost no painful feeling after surgery. Disadvantages include a complicated technique and a high risk of intraoperative complications.
Abdominal surgery
In order to gain access to the uterus during abdominal surgery, the surgeon makes an incision in the abdominal wall. After completing all stages of the hysterectomy, the doctor sews up the hole and applies a sterile, clean bandage.
Despite the fact that this type of removal is used quite often, it has a number of disadvantages.
Among them: significant trauma for the patient, a large scar on the abdomen, which remains after this type of surgery to remove the female reproductive organ.
The duration of this type of hysterectomy is approximately 40 minutes to 2 hours.
Laparoscopic
Gentle hysterectomy is a laparoscopic method of performing the intervention.
This type of surgery is performed without significant incisions on the abdomen.
To perform laparoscopic surgery, medical instruments and devices are used:
- First, gas is injected into the abdominal space through a gynecological tube called a cannula. This is required so that the wall of the peritoneum rises above the organs, and the surgeon has access to the organ to be removed.
- Then the surgery itself begins. In order to remove the uterus itself or other nearby organs, the surgeon inserts tubes into the abdominal space through small incisions on the abdomen. Through which a video camera and surgical devices are lowered into the cavity.
Laparoscopic excision of the uterus lasts 1.5-3.5 hours. The property of this method is that the incision is small, and accordingly there are no consequences in the form of a scar on the stomach.
Vaginal
The manipulation is a convenient option, does not require sutures, and does not leave scars. This type of hysterectomy is characterized by rapid physical and mental recovery.
Despite the many advantages, this type of surgery has a number of contraindications.
The operation is prohibited when:
- The uterus is of significant volume;
- A neoplasm of a malignant nature is present;
- There is an inflammatory phenomenon;
- Previous cesarean section;
- Associated diseases have been identified.
What is uterine laparoscopy and its advantages
Laparoscopic hysterectomy (removal) is a surgical method that allows manipulation through several small (5-10 mm) incisions. The following procedures can be performed using this method:
- conservative myomectomy (remove the myomatous node, preserving the uterus);
- supravaginal ectomy (remove the body without laparoscopy of the cervix);
- extirpation (laparoscopy of the uterus and appendages).
Abdominal abdominal surgery is certainly inferior to laparoscopic manipulation in the following areas:
- Safety. High-quality endoscopic equipment allows surgeons to perform complex manipulations without the risk of injury to important adjacent structures of the operated field.
- Fewer complications during and after laparoscopy. During the intervention, healthy tissues are minimally damaged, and the likelihood of secondary infection and the occurrence of reactive inflammatory complications is minimized.
- After laparoscopy, patients experience much less pain. This is due to the absence of a large wound surface. In addition, there is much less pain, since muscle structures are preserved during such an intervention.
- Facilitated postoperative care. Single skin sutures remain at the sites where endoscopic equipment is inserted, so after surgery, patients do not require special care and are discharged from the hospital much faster than during abdominal operations.
- More attractive total cost. Despite the fact that laparoscopic intervention may initially cost more than abdominal surgery, due to the short period of hospitalization and further recovery, the overall cost of such a procedure is significantly reduced.
Laparoscopic extirpation of the uterus and appendages can significantly reduce the rehabilitation period. The patient can be discharged from the medical facility within 7-10 days.
Anesthesia
For the most part, endotracheal joint anesthesia is used.
Many patients testify that it is well tolerated and does not cause headaches. The patient is awakened after 15-20 minutes, immediately after performing a similar operation, such as laparoscopic removal of the uterus.
Postoperative time with appropriate anesthesia leads to excellent results after surgery: there is no painful sensation, there is a slight inconvenience that disappears after 2 days. In some cases, nausea may occur, but this can be eliminated by Metoclopramide.
For the first 24 hours, you are allowed to drink only water. By the evening of the day of surgery, you can already rise and stand on your feet. The next day, you can eat food that slightly irritates the gastrointestinal tract: liquid cereals, meat broths, fermented milk products.
Discharge takes place on the second day after the amputation, and the sick leave ends after 30 days. After which the woman can go to work without difficulty, but with a restriction of heavy physical activity for 30 days.
The sutures are removed on the 5th postoperative day.
After surgery, complications are possible, which occur extremely rarely: injury to nearby organs by the trocar, bleeding from incompletely ligated veins, subdermal emphysema.
All this can be prevented if you strictly follow the technique of the event and carefully carry out visual inspection of the abdominal space.
Preparing for surgery
From reviews of women who underwent laparoscopic hysterectomy, it is known that patients are dissatisfied only with the preparation: the operation lasts 40 minutes, and preparation takes 2 weeks or more.
A woman should come to the operation after tests have been taken and the results have been received:
• blood tests (general, biochemical, blood group and Rh factor, hepatitis, syphilis and HIV, coagulability, glucose determination);
• urine tests - general and for sugar determination;
• strokes;
• electrocardiograms;
• fluorography;
• Ultrasound;
• colposcopy;
• examination by specialists: a therapist, if necessary a cardiologist, etc.
Before surgery, patients with uterine fibroids require separate diagnostic curettage of the uterus and obtaining histological results. This is necessary to resolve the issue of the scope of surgical intervention and to exclude and prevent the further development of oncological processes.
All examinations are a necessary procedure, and only after a complete examination will the surgeon be able to remove the uterus using the laparoscopic method.
The day before surgery, it is not recommended to eat, and you must shave your pubic hair.
Before the operation, the woman fills out a consent form for anesthesia and separately for the operation. If necessary, medication or psychoprophylactic preparation for surgery is carried out.
Operation duration
The duration depends on the method of admission, the type of excision and the volume of surgical intervention, the presence of adhesions, the volume of the uterus and a large number of other factors. However, the average duration of the entire operation is usually 1-3 hours.
The basic technical principles of intervention to remove the uterus with laparotomy and laparoscopic access are the same.
The fundamental difference is that in the first case, the organ with or without appendages is removed through an incision in the abdominal wall, and in the second, the organ is removed using an electromechanical device (morcellator) and is distributed in the abdominal space into parts, which are then removed using a laparoscopic tube (tube). ).
Progress of laparoscopic surgery
Laparoscopic surgery is performed under general anesthesia. After a small (3-4 mm) incision in the anterior abdominal cavity, special optical equipment and endoscopic surgical instruments are inserted into it. In addition, the abdominal cavity is filled with a certain amount of carbon dioxide.
After a laparoscope is inserted into the abdominal cavity, an inspection of the organs subject to surgical intervention is carried out. Then the surgeon cuts off the uterus, ligates the main vessels that supply it with blood, and, if there are medical indications, removes the uterine cervix and appendages. The amputated organs are then removed from the peritoneum by making an incision in the lower abdomen.
In particularly severe cases, there is a need to remove not only the body, cervix and appendages, but also the upper part of the vagina, as well as nearby lymph nodes and tissue fragments. Thus, gynecological organs are completely removed by laparoscopy only if there is a high probability of metastases spreading to adjacent pelvic organs.
Postoperative period
It is no secret that the time interval that lasts from the day of surgical removal until the restoration of work capacity and excellent health is called the postoperative period. Hysterectomy is also characterized by such a period.
The time after amputation is divided into 2 “sub-periods”:
- Early;
- Late postoperative period.
During the early postoperative period, the patient is in a hospital setting under the supervision of doctors. Its duration is related to surgical admission and the general condition of the patient after surgery.
After a hysterectomy of the uterus and/or appendages, which was performed either by an incision in the vagina or through an incision in the abdominal wall, the patient stays in the women’s department for 8–10 days, and it is at the end of this period that the sutures are removed.
After laparoscopic surgery to remove the uterus, the patient is discharged after 3 to 5 days.
The first day after surgery
The initial postoperative days are especially sensitive:
- Pain syndrome - at this time the patient feels significant pain both inside the abdominal cavity and in the location of the sutures, which is normal, since a wound has been formed both outside and inside (it is worth remembering what pain is like when an unintentional cut of a finger occurs). In order to eliminate painful manifestations, non-narcotic and narcotic painkillers are indicated.
- The legs and feet remain , as before the operation, in compression stockings or tightly bandaged with elastic bandages (to prevent the occurrence of thrombophlebitis).
- Activity - surgeons in almost all cases practice active management of the patient after the intervention, which means early getting out of bed (following laparoscopy after several hours, following laparotomy after 24 hours). Motor activity “gets the blood flowing” and ensures the functions of the gastrointestinal tract.
- Diet - the first day after hysterectomy, a gentle diet is recommended, which includes broths, pureed food and liquids (unsaturated tea, mineral water without gases, diluted natural juices). Such a therapeutic table non-aggressively promotes intestinal motility and helps early (1-2 days) spontaneous bowel movement. Self-emptying indicates normalization of the gastrointestinal tract, which entails a transition to the food the patient usually consumes.
- The abdominal cavity after surgery remains painful for 3–10 days, which is associated with the patient’s pain level. It is necessary to understand that the more active the patient behaves in the postoperative period, the sooner her general well-being is restored and the risk of possible complications decreases.
Treatment after surgery
Treatment after surgery is as follows:
- Antibiotics - as usual, antibacterial treatment is prescribed as a preventive measure, since the patient’s internal organs at the time of the operation were in contact with the environment, and therefore with all kinds of infectious pathogens. The duration of taking antibiotics lasts approximately a week;
- Blood thinners - by analogy, in the initial 2 - 3 days, anticoagulants (medicines that make the blood thinner) are indicated, which are aimed at protecting against thrombosis and the occurrence of thrombophlebitis;
- Parenteral infusions - on the initial day after hysterectomy, infusion treatment is carried out (intravenous infusion of compounds through a dropper) to compensate for the volume of circulating blood, since the operation is almost always associated with large blood loss (the amount of blood loss during hysterectomy without complications is 400 - 500 ml).
The early postoperative period is considered normal when there are no complications.
Consequences
It should be noted that after an operation such as laparoscopic hysterectomy, the consequences are usually minimal. Recovery occurs after 2 weeks of rehabilitation. 30 days after the operation, the woman can go about her usual activities. Vigorous physical exercise is recommended. But even after a month, it is undesirable to load the abdominal muscles, lift weights, or be in the sun.
In the first days, minor nagging pain in the lower abdomen is possible. This is normal and should go away in 1-2 days. The formation of an adhesive process is possible, but according to statistics, this occurs extremely rarely and only with a genetic predisposition of the body or with severe endometriosis.
Minor discharge from the genital tract is possible. This is normal if the ovaries are preserved. They continue to produce hormones that cause this reaction.
Cases of inflammatory processes after laparoscopic operations are rare, because antibiotic therapy is prescribed immediately after the intervention and continues for 5 days. At the same time, the water-electrolyte composition of the blood is corrected.
The patient's fertility is restored almost immediately, and in some cases there is even an increase in libido. A woman can be sexually active 1 month after surgery. If the organ is preserved, you can become pregnant six months after the intervention.
Recovery and rehabilitation
The rehabilitation and recovery time after surgery to remove the uterus is the most difficult when it comes to abdominal surgery. Postoperative time is presented as a week, and the sutures from the scar are removed on the sixth or seventh day.
Abdominal or abdominal surgery to remove the female reproductive organ is required for uterine cancer, significant fibroids, or in situations of suspected ovarian cancer.
Such a surgical intervention makes it possible to more accurately assess the degree of disease of the genital organs, but it increases and aggravates the recovery time after excision of the reproductive organ.
The method of vaginal removal of a diseased organ is practiced by cutting the deep walls of the vagina. The patient at this moment is located in the gynecological chair.
Such a surgical procedure is carried out in the absence of the slightest suspicion of any form or type of oncology, and when the uterus is small. Vaginal ectomy is complicated by the fact that it is performed blindly and for this reason, the occurrence of postoperative health complications becomes likely.
Nutrition
The patient’s diet after surgery to remove the uterus must include the principle of a gentle regime: the exclusion of aggressive or irritating foods to the mucous membrane of the gastrointestinal tract.
The following foods must be avoided:
- confectionery products,
- rich coffee and tea,
- cheese and cottage cheese,
- chocolate,
- white bread, buns.
To “start” intestinal functions after surgical manipulation, you need to eat in small portions, but often - 5-7 times a day. The daily volume of water consumption must be increased to 2-4 liters.
The consumption of foods that have a laxative effect is required: all types of cereals, meat and vegetable broths, fermented milk products.
The main instruction is to strictly follow the diet prescribed by the attending physician, both in the initial days after the end of the operation and during the rehabilitation period.
Physical exercise
Operated patients are prohibited from lifting large bags or other heavy items for about a month and a half after discharge from the hospital. The timing is similar for the start of sexual activity.
Visiting the pool for women who have undergone surgery to remove the uterus is permissible no earlier than 6-8 weeks after hysterectomy.
Despite the fact that the sutures dissolve in the body within 6 weeks, surgeons recommend starting physical exercise or going to a fitness center only six months after abdominal surgery, when a scar has formed. The patient’s leading specialist will explain a lot about light exercise classes.
Operation technique
Surgery to remove the uterus using the laparoscopic method is performed for fibroids up to 16 weeks of pregnancy, which are complicated by bleeding, characterized by rapid growth or the risk of malignant degeneration. Although some experienced specialists completely remove the uterus, the size of which is about 20 weeks. But most often, given the woman’s age, uterine fibroids are removed laparoscopically, leaving a small part of the uterus for menstruation.
Three or four punctures are used in the abdominal wall (one near the navel, the other two on the sides) and trocars are inserted. This is a device equipped with a monitoring camera or light installation with a carbon dioxide or nitrous oxide blower and tools.
After examination, uterine fibroids are removed laparoscopically. To do this, the ligaments are excised, the vessels are ligated, the uterus is cut off from the vaginal walls and removed through the vagina through incisions in the fornix. This operation is called laparoscopically assisted vaginal myomectomy. The incisions in the vagina are sutured. In one operation, it is possible to remove several nodes without repeated intervention.
At the end, the blood or fluid that accumulated during the operation is removed, and the organs and walls of the abdominal cavity are examined again. Carefully check whether the vessels are well ligated and ligated, and whether there is any leakage of blood or lymph fluid. Eliminate the gas and remove the instruments. Then sutures are placed on the skin and subcutaneous tissue at the sites where the trocars are inserted, and the skin is sutured with cosmetic sutures.
The duration of the operation can be from 15 minutes to 1.5 hours, depending on the volume of surgery performed.
Doctors' recommendations
After the intervention, the period of bringing the body back to normal and recovery becomes very important, so each woman receives the necessary recommendations from a gynecologist or surgeon, which will provide a preventive option against the occurrence of complications, will quickly recover and return to normal after the operation.
Among the fundamentally important tips, the following become mandatory:
- Sex after surgery to remove the uterus can be no earlier than after 2 months. Moreover, during sexual intercourse, a woman should not feel pain or discomfort;
- To ensure the avoidance of difficulties with urination, Kegel exercises;
- It is imperative to consult with a specialist regarding the use of medications to prevent diseases in bone tissue;
- It is important to strictly follow the diet;
- Spend a lot of time in clean air.
The attention and care of loved ones undoubtedly contributes to rapid rehabilitation.
When a woman, after an operation, is subject to psycho-emotional depression and is not able to overcome her own difficulties on her own, she needs outside help in the form of psychological recovery, conversations with a psychologist, and most importantly, the care and love of family members.
The hysterectomy slightly changes the patient’s usual lifestyle.
In order to ensure a quick and successful recovery and recovery after surgery, doctors inform their patients about rehabilitation methods and specific steps on the path to recovery.
Postoperative bandage
If the early postoperative period proceeded without any negative changes, then after the patient’s stay in the hospital has passed, she should immediately take care of her own health and prevent future consequences.
The bandage is a very good helper for her in this matter.
This device is a help during the final postoperative period. It is especially acceptable for those women who are classified in the premenopausal age category and have a history of numerous pregnancies and childbirths with aggravated conditions.
There are a number of models of such a support corset; it is necessary to select only the option in which a woman who has undergone surgical surgery does not feel any discomfort or inconvenience.
The main condition when selecting a corset bandage is that its width boundaries must be located higher than the scar, at least 100 mm above and below (in the event that a laparotomy was performed in the area below the middle of the abdomen).
Contraindications
The laparoscopic method is not used in the following cases:
- The uterus measures more than 16 weeks even after treatment with gonadotropin-releasing hormone agonist drugs.
- Uterine prolapse. In this case, the optimal access is vaginal.
- Ovarian cystomas, that is, cysts whose size is more than 8 cm in diameter. Such fluid-filled formations cannot be removed through a small laparoscopic incision without making punctures. But this formation cannot be pierced: it may contain cancer cells, and due to the puncture they can get into the peritoneum and internal organs and grow into them.
- The presence of fluid in the abdomen in a volume of more than 1 liter (in this case, laparotomy surgery is required).
- Many adhesions in the abdominal cavity that surround the intestines.
- Obesity.
- Impaired blood flow in the brainstem area (vertebrobasilar insufficiency).
- Diaphragmatic hernia.
Pros and cons of the operation
Positive aspects still exist after surgery to remove the uterus. Before deciding on this surgery to excise the uterus with or without appendages, you need to soberly evaluate all the advantages and disadvantages.
The positive properties of hysterectomy include:
- absence of menstrual flow and, along with it, the question of the need to use protective equipment;
- absence of pain and bleeding , which significantly complicated the quality of life;
- guarantee against uterine cancer (no organ – no threat), weight loss, waist reduction.
The negative points include:
- psycho-emotional disorders;
- scar below the abdomen;
- the duration of the painful syndrome in the postoperative period is 3 – 6 – 12 months;
- fulfillment of the condition of sexual rest lasting 1.5 – 2 months;
- more untimely (early) onset of menopause;
- the risk of osteoporosis and heart disease is 5 years earlier than in women who have not undergone surgery.
Indications and contraindications
Indications
- uterine fibroids, accompanied by pain, bleeding, dysfunction of the intestines and urinary system;
- adenomyosis of the uterus with pain and bleeding;
- emergency situation (bleeding, disseminated intravascular coagulation syndrome);
Contraindications
- inflammatory processes of any localization in acute form;
- background and precancerous diseases of the cervix;
- recurrent form of endocervical disease;
- anemia.
Uterine artery embolization - as an alternative
Uterine artery embolization is perceived as an innovative and modern technology, despite the fact that it began to be actively used back in the 70s of the 20th century.
The principle of embolization is presented in the form of inserting a catheter into the femoral vein, then the tube reaches the uterine vein (under observation by means of radiography), and then the area where the arteries and veins branch from it, which provide blood supply to the fibroid nodes.
The introduction of specially created medications through a catheter creates a blockage of blood supply in small capillaries, leading to myomatous neoplasms and disrupts blood circulation in them.
Embolization of the uterine arteries is becoming an excellent option for replacing surgery to remove uterine fibroids, since it helps stop the growth and development of nodes, and even minimize their size or completely dry out.
A similar manipulation is carried out in the presence of developing uterine fibroids up to 20 weeks, but in cases where pathologies of the ovaries and cervix are not observed, and in patients who are infertile due to the development of fibroids.
In addition, uterine artery embolization is prescribed for uterine bleeding, which can cause the patient’s death.
And yet, situations arise when a hysterectomy due to fibroids becomes impossible to replace in any other way:
- submucosal uterine fibroids;
- significant volumes of uterine fibroids;
- aggravation of fibroids by the growth of the inner layer of the uterus and neoplasms of the ovaries;
- continuous bleeding, which can lead to iron deficiency and anemia;
- developing and growing neoplasm.
In which cases?
At its core, embolization of the reproductive organ and nearby tissues is prescribed when the following signs and conditions appear:
- In the case when the fibroid tumor is no more in size than the 12-week state of pregnancy;
- In circumstances where a woman plans to become pregnant in the future, and for this reason she requires preservation of her reproductive organs;
- When establishing contraindications to surgical procedures, narcotic or non-narcotic painkillers, etc.;
- In a situation where, after surgical removal of the node, the fibroid resumed its growth and development;
- Presence or threat of endometriosis;
- Postpartum blood loss;
- In circumstances where accelerated growth of a neoplasm, etc., has been established.
Similar to any medical procedure, surgical manipulation to remove the uterus has characteristic contraindications such as:
- The size of fibroid formations is too large, when the uterus is enlarged in size when compared with the 25-week state of gestation;
- The presence of a large number of neoplasms of different sizes;
- Inflammatory vaginal diseases;
- Insufficient kidney function;
- The state of bearing a child;
- Myoma blood supply disorder;
- Presence of parallel oncology of the external genital organs, etc.
As usual, if there are contraindications, venous occlusion is performed, which is performed using the laparoscopic method.
In some cases, occlusion has only a temporary property; it is in such a situation that the blood supply is blocked for a certain time interval, thanks to specially created blood clots, gelatin-containing medications and other devices and components. Still, temporary occlusion is used quite infrequently.
What is the uterus and what function does it perform?
The uterus is a reproductive organ in the female body that is responsible for procreation. In its structure, the organ resembles a small bag, which is covered with elastic muscles. Typically, the main function of the uterus is to carry the fetus from conception to birth. Just like other organs, the pyriform hollow body is nourished by blood vessels. Despite popular belief, the organ is not responsible for the production of hormones, such as the ovaries, thyroid gland and pituitary gland, but is important for those who want to bear a healthy baby.
Note. The uterus is a capricious organ that can easily become dislodged if the body is subjected to excessive stress. It is for this reason that a woman is not recommended to lift weights of more than 2 kg in one hand. There are also pathologies (defects) of this organ, for example prolapse, prolapse or duplication.
Consequences and complications
After removal of the uterus, the following complications may occur:
- Painful sensation after hysterectomy surgery may be due to the formation of adhesions or blood loss. These signs quite often occur on the first day after the operation.
- In addition, the consequences of the intervention may include thrombosis of the deep vessels of the legs , all kinds of urination disorders, fever, suppuration and inflammation of the stitching site, bruises and extensive hematomas.
- In addition, a decrease in the degree and strength of sexual desire and the occurrence of dryness in the vaginal cavity are likely, however, such complications are more an exception than an axiom.
- Women after surgery become significantly prone to such pathologies as osteoporosis and atherosclerosis.
All these complications and negative manifestations significantly lengthen the time of rehabilitation and recovery. Quite often, after removal of the uterus, women experience all the signs and symptoms of menopause.
Complications after laparoscopy of uterine fibroids
Most often, laparoscopy of uterine fibroids is very easy and problem-free for the patient. But sometimes various complications occur. Let us list the main signs that should alert a woman.
- Prolonged pain in the pelvic area, in which standard painkillers are ineffective.
- General weakness and loss of strength.
- Heavy, prolonged bleeding from the vagina.
- High temperature after laparoscopy of uterine fibroids.
Cost of the operation
Unambiguously answer the question “what is the cost of this operation?” very difficult. Often the cost depends on many reasons.
Among the main ones:
- area of permanent residence of a woman,
- class of hospital and specialists,
- scale of hysterectomy and its duration,
- hospital conditions.
Further, the cost of amputation is influenced by the type of surgical procedure chosen by the surgeon based on the woman’s condition.
For example, laparoscopic extirpation in private medical institutions will cost the patient 16,000-90,000 rubles , and for the vaginal method of removing the reproductive organ you will have to pay in the region of 25,000 to 85,000 rubles.
Where can the operation be performed?
Many medical institutions can offer laparoscopic hysterectomy. In Moscow, city hospitals that are equipped with equipment and have specialists proficient in this technique will offer you these services. The price of the operation is discussed with the attending physician.
The examination can be carried out in the department itself or previously in the hospital at your place of residence. To carry out such operations, it is possible to issue a quota. The cost of laparoscopic hysterectomy ranges from approximately 45 to 70 thousand.
Benefits and risks of laparoscopy
The main advantages of laparoscopy are as follows:
- low tissue trauma;
- short rehabilitation period;
- lower costs of medications compared to laparotomy;
- reducing the load on the body;
- minimum period of hospitalization;
- organ preservation;
- reducing the risk of adhesions.
Despite the apparent advantages, laparoscopy has its disadvantages. During surgery, there remains a high risk of internal bleeding, which is difficult to stop using laparoscopic access. Then surgeons are forced to complete the operation by performing a laparotomy. After removal of myomatous nodes, scars remain on the uterus, which can pose a threat to the fetus and mother during childbirth. The possibility of developing an adhesive process remains.
These problems do not occur in patients undergoing uterine artery embolization by our endovascular surgeons. Since the embolic agent is introduced into the uterine arteries by puncture of a peripheral vessel, internal bleeding cannot develop a priori. After embolization, the fibroid nodes are replaced by connective tissue, and scars on the uterus are not formed. The surgeon does not manipulate the abdominal cavity, so adhesions do not develop in it.
Possible complications
Laparoscopy of the uterus is a relatively gentle manipulation, but complications are not excluded:
- damage to large vessels, which is recognized by severe bleeding.
- subcutaneous emphysema (accumulation of air in the subcutaneous tissue);
- mechanical damage to internal organs;
- formation of hematomas at puncture sites;
- development of inflammation against the background of secondary infection.
Minor bloody vaginal discharge after a hysterectomy is normal and usually goes away on its own within 2-3 weeks. If the appendages were also removed, then in the near future after the operation the woman may experience symptoms that usually occur during menopause (hot flashes, hyperhidrosis, sleep problems, emotional instability).
If you refrain from hormonal therapy, which will simulate the work of the female reproductive glands, then after some time pathologies of the cardiovascular system may arise, inflammation of the bladder, dryness and itching of the vagina will often begin to bother you.
When the reproductive organs are removed, a woman certainly loses her reproductive abilities, but this is an extreme measure, which in many cases can save her life. The laparoscopic method of extirpation not only allows this procedure to be performed with less damage to health, but also aesthetically it causes women much less inconvenience.
For many years, gynecologists have suggested removing the uterus to treat uterine fibroids. There are alternative treatment methods that can get rid of the disease and save the organ.
Please note that this text was prepared without the support of our Expert Council.
We work with fibroid clinics where doctors treat uterine fibroids by performing uterine artery embolization. This is a procedure that does not require any skin incision. After it, there are no scars left either on the uterus or on the abdomen. Myomatous nodes decrease in size, most of them disappear. After embolization of the uterine arteries, no relapse of the disease is observed.
If you have been diagnosed with uterine fibroids, there is no need to worry. Call. You will be given an appointment with a gynecologist, examination and treatment will be organized in the best gynecological clinics. Our staff will accompany you at all stages of diagnosis and treatment. They will help you in solving all organizational issues. You always have the opportunity to get expert advice by e-mail.
Doctors widely use laparoscopy to diagnose and treat gynecological diseases. This is a minimally invasive surgical intervention that allows the gynecologist, after inserting a manipulator with a video camera into the abdominal cavity, to obtain an image of the internal organs on the monitor. It is used to determine the location and size of myomatous nodes. During the operation, the surgeon has the opportunity to collect pieces of tissue for histological examination. Laparoscopy of the cervix can identify fibroids or other pathological formations.
Diagnostic laparoscopy of the uterus is performed in the presence of acute surgical pathology of the abdominal cavity. Using this method, the cause of infertility is determined. Quite often, after diagnosing the disease, the surgeon proceeds to the main stage of the operation. He removes myomatous nodes, dissects adhesions in the pelvis and abdominal cavity. Laparoscopy of the uterus is an organ-preserving method of treating fibroids.
Medical contraindications
Laparoscopic extirpation (removal) of the uterus is contraindicated in the following cases:
- acute blood loss due to hemodynamic instability;
- the danger of tumor rupture into the peritoneum during its resection;
- the size of the uterus, as at 16 weeks of pregnancy (for large fibroids);
- prolapse due to uterine prolapse (vaginal access is recommended);
- abdominal ascites (fluid more than 1 liter);
- adnexal cystomas;
- general serious condition of the patient;
- decompensated chronic diseases.