What is hysteroscopy with RDV
RDV in decoding is called separate diagnostic curettage. It is done if there are suspicions of pathological processes inside the uterus or if the disease progresses. RDV is a surgical procedure, a process separate from hysteroscopy. It is performed to examine the cavity using a special device.
When combined, both procedures received a new name - RDV hysteroscopy. That is, during the examination, tumors can be removed and scrapings taken from different places. Thanks to hysteroscopy with RDV, the samples taken help determine the nature of the formations and carry out more precise removal of individual elements.
Indications for the procedure
Indications for RDV are a number of pathological processes in the uterine cavity, based on the patient’s complaints, ultrasound data and examination by a gynecologist, when more accurate data is required to make the correct diagnosis. The operation is also prescribed for:
- infertility;
- the presence of intrauterine septa;
- inability to bear a child;
- oligomenorrhea;
- very heavy menstruation;
- suspicion of fibroids, hyperplasia, perforation of the uterine walls;
- sudden bleeding;
- the appearance of discharge during menopause;
- assessment of the condition of the uterus.
The therapeutic option of hysteroscopy with RDV is prescribed:
- if you suspect cervical or endometrial cancer;
- after early miscarriages;
- in case of synechia (fusion of cavity walls);
- for verification of endometriosis;
- when cleaning is required after an abortion or miscarriage;
- for the diagnosis of uterine malformations.
Hysteroscopy with RDV is performed after gynecological operations. Performed in combination with conventional diagnostics - to remove polyps, separate adhesions, and remove small tumors.
Which female organ is curetted?
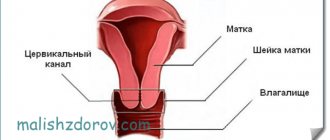
The uterus is scraped out. This is a hollow pear-shaped organ, in which there are three sections:
- body – the largest part;
- isthmus – located between the body and the neck;
- The cervix is the narrowed lower end of the uterus.
The uterine wall has three layers:
- inner layer (mucous) – endometrium;
- the middle layer is represented by smooth muscle tissue (myometrium);
- the upper layer is serous (perimetry).
The uterus performs important functions:
- childbearing;
- menstrual;
- participates in the birth act.
The endometrium is cleaned. Its peculiarity lies in the fact that every month every non-pregnant woman of childbearing age experiences a rejection of the functional layer, which manifests itself in the form of menstrual bleeding. Before this, it thickens several times, thereby preparing to receive a fertilized egg.
It is important for every woman who is scheduled for curettage to understand the following: as part of this procedure, only the functional layer of the endometrium is removed, which itself is rejected physiologically in each cycle. After the intervention, the mucous tissue is restored.
Along with the endometrioid tissue, neoplasms (if any) are also removed: polyps, intrauterine adhesions, etc.
Contraindications
The procedure is not performed if a malignant tumor is detected in the cervical canal. Despite the fact that RDV hysteroscopy is a minimally invasive surgical method, it also has a number of other contraindications:
- severe somatic diseases;
- inflammatory pathologies of the genitourinary system;
- a large tumor in the uterus or on its cervix;
- serious heart disease;
- stenosis of the cervical canal;
- 3-4 degree of vaginal cleanliness;
- diseases of the thyroid gland and internal organs;
- successful pregnancy;
- infectious pathologies in acute form (flu, pneumonia, sore throat, etc.);
- constant bleeding from the genitals.
Contraindications can be absolute or temporary. The last group includes inflammatory diseases and stenosis of the cervical canal. Then RDV with hysteroscopy is performed without dilation of the uterine cervix, and other gynecological manipulators are used during the operation.
For inflammation, 3-4 vaginal cleanliness, infectious pathologies, preliminary treatment is carried out before the procedure. Uterine bleeding is not an absolute contraindication. However, curettage and assessment of the uterine cavity will not be informative enough. Absolute contraindications include only chronic cardiovascular pathologies, serious diseases of the kidneys, liver and lungs, and normal pregnancy.
Progress of the Russian Far East
Diagnostic curettage of the uterine cavity is performed in the operating room. It is best to do the procedure 3-4 days before menstrual bleeding. This is the most favorable period for curettage. In case of bleeding from the uterine cavity - immediately after diagnosis.
In terms of time, the RDV of the uterus lasts no more than half an hour. It is performed under anesthesia - local or general. When choosing a local anesthesia, the cervix is punctured. In the second case, the medicine is administered intravenously.
To avoid infection, the vulva and cervix are treated with an aqueous solution of alcohol or iodine. The doctor needs to expose the cervix using a speculum, after which he hooks and fixes it. Then it enters the cervical canal with a special probe, penetrates the cavity and measures its depth. After this, you can proceed to dilation of the cervix. Expanders - metal sticks of different thicknesses - are inserted into the canal one by one. The cervical canal gradually increases and reaches a size capable of passing a curette, with the help of which curettage occurs. This tool resembles a spoon with a handle and one sharpened edge.
The operation takes place in 2 stages:
- scraping the mucous membrane of the cervical canal of the cervix without penetrating into the internal cavity;
- curettage of the internal cavity of the uterus.
The mucous membrane of the cervix is scraped out with the smallest curette.
If diagnostic curettage of the uterine cavity is carried out together with hysteroscopy, then after dilation of the cervical canal, a hysteroscope is inserted into the cavity and an examination is performed. Then curettage of the uterine cavity is performed. Some formations cannot be removed in this way. Then you have to use special instruments, they are inserted into the cavity and then the formations are removed.
In order to make a diagnosis, scrapings of the mucous membrane are placed in containers and then sent for histological or other analysis.
At the end of the diagnostic separate curettage, the patient, who has no visible complications, can be sent home after 3-4 hours. A follow-up examination and ultrasound should be performed after a week.
Preparation
Before hysteroscopy with RDV, the patient undergoes tests and instrumental examinations. Blood tests are taken - general and biochemistry, OAM, vaginal smears, determination of glucose levels. Blood is checked for hepatitis, HIV, syphilis. Results last only for ten days. From instrumental studies the following is prescribed:
- coagulogram;
- fluorography of the lungs;
- ECG with interpretation;
- Ultrasound of the pelvis and vagina.
Since the operation is performed on an empty stomach, you can eat your last meal 12 hours before the operation. If the patient has varicose veins, then the legs are first bandaged with an elastic bandage or compression garments are put on. This is necessary to reduce the risk of thrombosis. Before the procedure, the woman is examined in a chair by a gynecologist. In the morning before the operation, the bladder is emptied, hair in the genital area is shaved, and the genitals are washed thoroughly. An anesthesiologist is examining you in the office.
Pregnancy and childbirth after curettage of the uterine cavity
The first menstruation after curettage may occur with some delay (in some cases up to four weeks or more), which is associated with hormonal imbalance.
This is also considered normal after curettage. You should sound the alarm if your period does not come for more than two months - this is a serious reason to consult a gynecologist.
In general, most women get their period within two to three weeks, which means that in the new cycle (i.e., with the arrival of their period), there is theoretically a chance of becoming pregnant.
Childbirth after the procedure usually proceeds well.
If a woman tries to conceive a child for six months or more after curettage, but there are no results, it is necessary to undergo additional examination by a gynecologist. Curettage should not negatively affect fertility; on the contrary, this procedure is often performed as part of the complex treatment of infertility.
The pregnancy planning plan after curettage is built depending on what caused the need for the operation. If a woman sets a goal to become pregnant after curettage, she must inform her gynecologist about this. The specialist will give an adequate assessment of the situation and recommend the timing of pregnancy planning.
Carrying out
Hysteroscopy with separate diagnostic curettage is performed 5-10 days after the start of menstruation (this occurs during hormonal imbalances). If there is a suspicion of cancer, then on any day, if non-ovulation cycles are diagnosed - 2-3 days before menstruation. If uterine bleeding is observed, then only after it stops. The operation is carried out in several stages:
- First, the patient undresses, lies on the operating table, and is given anesthesia. Anesthesia is selected depending on the patient’s age, her state of health, and current chronic pathologies. Anesthesia can be general and local. In the latter case, the patient remains conscious, but does not feel pain.
- The uterine cervix is dilated using gynecological instruments. This is necessary for unhindered penetration of manipulators into the cavity. The perineum and genitals are treated with a disinfectant. Speculums are inserted into the vagina and the cervix is fixed with forceps.
- The internal surface of the uterine cavity and its cervix is visually assessed. This helps to create an overall picture of pathological changes. One mirror is removed, the other is held by a nurse. RDV is carried out using a curette. For this purpose, expansion of the cervical canal is used, which is carried out using instruments and liquid. First, tissue is taken from the inner wall of the cervix, then the uterus.
- Samples are sent to the laboratory for testing. The neck is filled with iodine.
The operation lasts from 15 minutes to half an hour, so only short-term anesthesia is administered, which allows you to quickly return to normal life. From several hours to a day, the patient should remain in the hospital, under the supervision of a doctor.
Lecture “How to avoid becoming a victim of a gynecologist”
Most women in their lives are faced with a situation where the gynecologist, after an examination, prescribes curettage. “cleaning” among themselves
Not all patients are told in an accessible form what this operation is, and this ignorance gives rise to unfounded worries.
Let's figure it out
.
- What is scraped out (a little anatomy)?
- Explanation of names
- Why is curettage performed?
- What preparation for curettage
- How does scraping happen?
- Complications of curettage
- What's next?
What is scraped out (a little anatomy)?
The uterus is a muscular organ shaped like a “pear”, in which there is a cavity that communicates with the external environment through the cervix, which is located in the vagina. The uterine cavity is the place where the fetus develops during pregnancy. The uterine cavity is lined with mucous membrane (endometrium). The endometrium differs from other mucous membranes (for example, in the oral cavity or in the stomach) in that it is capable of attaching a fertilized egg to itself and giving rise to the development of pregnancy.
During the entire menstrual cycle, the lining of the uterus (endometrium) thickens, various changes occur in it, and if pregnancy does not occur, it is rejected in the form of menstruation and begins to grow again in the next cycle.
During curettage, it is the mucous membrane of the uterus - the endometrium - that is removed, but not the entire mucous membrane is removed, but only the superficial (functional layer). After curettage, a germinal layer of the endometrium remains in the uterine cavity, from which a new mucous membrane will grow.
For example, every autumn a rose bush is cut at the root and in the spring a new rose bush grows from this root. In fact, curettage is similar to regular menstruation, only performed with an instrument. Why this is done - read below.
During this operation, the cervical canal (the place where the entrance to the uterus is located) is also scraped. This is where the curettage procedure usually begins - the mucous membrane that lines this canal also down to the germ layer is scraped off. The resulting scraping is sent for examination separately.
Explanation of names
Scraping
- this is the main action during manipulation, but the manipulation itself can have different names.
Russian Far East
– separate diagnostic (sometimes an addition: therapeutic and diagnostic) curettage of the uterine cavity. The essence of this name: will be fulfilled
- separate
(first curettage of the cervical canal, then the uterine cavity) - treated-diagnostic
- the resulting scraping will be sent for histological examination, which will allow an accurate diagnosis to be made, “treated” - since in the process of curettage the formation (polyp, hyperplasia) for which it was prescribed is usually removed. - curettage
- description of the process.
RDV+ GS
– separate diagnostic curettage under hysteroscopy control is a modern modification of curettage. Conventional curettage is performed virtually blindly. When using hysteroscopy (“hystero” - uterus; scopia - “look”), the doctor inserts a device into the uterine cavity with which he examines all the walls of the uterine cavity, detects the presence of pathological formations, then performs curettage and finally checks his work. Hysteroscopy allows you to evaluate how well the curettage was performed and whether there are any pathological formations left.
Why is curettage performed?
Curettage is carried out for two purposes: to obtain material
(scraping of the mucous membrane) for histological examination - this allows for a final diagnosis; the second goal is to remove the pathological formation in the uterine cavity or cervical canal.
Diagnostic purpose of curettage
- If a woman’s ultrasound shows changes in the mucous membrane, ultrasound does not always allow an accurate diagnosis; most often we see signs indicating the presence of a pathological process. Sometimes ultrasound is performed several times (before and after menstruation). This is necessary in order to be sure that the pathological formation actually exists and is not just a variant of the structure of the mucous membrane only in this cycle (an artifact). If the formation that was found remains after menstruation (that is, rejection of the mucous membrane), then it is a true pathological formation, it has not been rejected along with the endometrium, curettage should be performed.
- If a woman has heavy, prolonged menstruation with clots, intermenstrual bleeding, pregnancy and other, rarer conditions do not occur for a long time, and according to ultrasound and other research methods it is not possible to establish the cause
- If there are suspicious changes on the cervix, a diagnostic curettage of the cervical canal is performed
- Before a planned gynecological operation
or procedure for uterine fibroids, in which the uterus will be preserved.
Therapeutic purpose of curettage
- Mucosal polyps (polyp-like growths of the uterine mucosa) - there is no other type of treatment, they do not disappear with medication or on their own (there will be a separate article on the site)
- The hyperplastic process of the endometrium (hyperplasia) - excessive thickening of the uterine mucosa - is treated and diagnosed only by curettage, followed by drug therapy or instrumental methods (there will be a separate article on the site)
- Uterine bleeding – the cause may not be known. Curettage is performed to stop bleeding.
- Endometritis is an inflammation of the uterine mucosa. For complete treatment, the mucous membrane is first scraped off.
- Remains of membranes and embryonic tissues - treatment of complications after abortion
- Synechia - fusion of the walls of the uterine cavity - is performed using a hysteroscope and special manipulators. Under visual control, adhesions are dissected
How to prepare for curettage?
If curettage is not performed for emergency reasons (as, for example, during uterine bleeding), but as planned, the operation is performed before menstruation, a few days before its onset. This is necessary so that the curettage process itself practically coincides in terms of the physiological period of rejection of the uterine mucosa (endometrium). If you plan to undergo hysteroscopy with removal of a polyp, the operation, on the contrary, is performed immediately after menstruation so that the endometrium is thin and the location of the polyp can be accurately seen.
If curettage is carried out in the middle of the cycle or at the beginning, this can lead to prolonged bleeding in the postoperative period. This is due to the fact that the mucous membrane of the uterus grows synchronously with the growth of follicles in the ovaries - if the mucous membrane of the uterine cavity is removed significantly before the onset of menstruation, the hormonal background created by the ovaries will “come into conflict” with the absence of the mucous membrane and will not allow it to fully grow . This condition is normalized only after synchronization between the ovaries and the mucous membrane occurs again.
It would be logical to propose curettage during menstruation, so that the natural rejection of the mucous membrane coincides with the instrumental one. However, they do not do this, because the resulting scraping will not be informative, since the rejected mucous membrane has undergone necrotic changes.
Tests before curettage (basic set):
- General blood analysis
- Coagulogram (assessment of the blood coagulation system)
- ECG
- Tests for hepatitis B and C, RW (syphilis) and HIV
- Vaginal smear (there should be no signs of inflammation)
On the day of curettage, you need to come on an empty stomach, the hair in the perineum should be removed. You bring a robe, long T-shirt, socks, slippers and pads.
How does curettage occur?
You are invited to a small operating room, where you sit on a table with legs, like a gynecological chair. The anesthesiologist will ask you about your previous illnesses and any allergic reactions to medications (prepare for these questions in advance).
The operation takes place under intravenous anesthesia - this is a type of general anesthesia, but only it is short-term, on average 15-25 minutes.
After the drug is injected into a vein, you immediately fall asleep and wake up in the ward, that is, you sleep throughout the operation and do not experience any unpleasant sensations, but on the contrary, you may have sweet dreams. Previously, heavy drugs were used for anesthesia, which caused very unpleasant hallucinations - now they are no longer used, although the skill of the anesthesiologist in administering anesthesia is of great importance.
The operation itself is performed as follows. The doctor inserts a speculum into the vagina to expose the cervix. Using special forceps (“bullet pins” there is a tooth at the ends of this instrument) it catches the cervix and fixes it. This is necessary to ensure that the uterus remains motionless during the procedure - without fixation, it easily moves, as it is suspended by ligaments.
Using a special probe (iron rod), the doctor enters the cervical canal and penetrates the uterine cavity, measuring the length of the cavity. After this, the stage of cervical dilatation begins. Extenders are a set of iron sticks of varying thickness (in ascending order from the thinnest to the thickest). These sticks are alternately inserted into the canal of the cervix, which leads to a gradual expansion of the canal to a size that freely passes the curette, the instrument used to perform curettage.
When the cervical canal is dilated, the mucous membrane of the cervical canal is scraped. This is done with the smallest curette. A curette is an instrument similar to a spoon with a long handle, one edge of which is sharpened. A sharp edge is used to scrape. The scraping obtained from the cervical canal is placed in a separate jar.
If curettage is accompanied by hysteroscopy, then after dilation of the cervical canal, a hysteroscope (a thin tube with a camera at the end) is inserted into the uterine cavity. The uterine cavity and all walls are examined. After this, the lining of the uterus is scraped. If a woman had polyps
– they are removed with a curette during the curettage process. After the curettage is completed, the hysteroscope is reinserted and the result is checked. If something remains, reinsert the curette and scrape it out until the result is achieved.
Some formations in the uterine cavity cannot be removed with a curette (some polyps, synechiae, small myomatous nodes growing into the uterine cavity
), then special instruments are inserted into the uterine cavity through
a hysteroscope
and, under visual control, these formations are removed.
After the scraping
Forceps are removed from the cervix, the cervix and vagina are treated with an antiseptic solution, ice is placed on the abdomen so that under the influence of cold the uterus contracts and the small blood vessels of the uterine cavity stop bleeding. The patient is transferred to the ward, where she wakes up.
The patient spends several hours in the ward (usually sleeping, with ice on her stomach) and then gets up, gets dressed and can go home (if this is not a day hospital, but a hospital, discharge is carried out the next day).
Thus, curettage occurs without any painful or unpleasant sensations for the woman
, takes about 15-20 minutes, the woman can go home the same day.
Complications of curettage
In general, curettage in the careful hands of a doctor is a fairly safe operation and is rarely accompanied by complications, although they do occur.
Complications of curettage:
- Perforation of the uterus
- the uterus can be perforated using any of the instruments used, but most often it is perforated with a probe or dilators.
Two reasons: the cervix is very difficult to dilate, and excess pressure on the dilator or tube causes it to pierce the uterus; Another reason is that the uterus itself can be greatly changed, which makes its walls very loose - because of this, sometimes the slightest pressure on the wall is enough to pierce it. Treatment:
small perforations heal on their own (observation and a set of therapeutic measures are carried out), other perforations are sutured and surgery is performed. - Cervical tear
– The cervix is most often torn when the bullet forceps fall off.
Some cervixes are very “flabby” and bullet forceps do not hold well on them - at the moment of tension, the forceps fly off and tear the cervix. Treatment:
small tears heal on their own; if the tear is large, stitches are applied. - Inflammation of the uterus
- this occurs if curettage was performed against the background of inflammation, the requirements of septic and antiseptics were violated, and a prophylactic course of antibiotics was not prescribed.
Treatment:
antibacterial therapy. - Hematometra
is an accumulation of blood in the uterine cavity.
If, after curettage, a spasm of the cervix occurs, blood, which normally should flow from the uterine cavity for several days, accumulates in it and can become infected and cause pain. Treatment
: drug therapy, bougienage of the cervical canal (spasm relief) - Damage to the mucous membrane
(excessive curettage) – if you scrape very hard and aggressively, you can damage the germinal layer of the mucous membrane, which will lead to the fact that the new mucous membrane will no longer grow.
A very bad complication - practically untreatable.
In general, complications can be avoided if this operation is performed carefully and correctly.
.
Complications of curettage include situations when, after this operation, the entire pathological formation (polyp, for example) or part of it remains in place. More often this happens when curettage is not accompanied by hysteroscopy
, that is, it is impossible to evaluate the result at the end of the operation. In this case, curettage is repeated, since it is impossible to leave the pathological formation in the uterine cavity.
What's next?
After curettage, you may have spotting and spotting for several days (from 3 to 10). If the bleeding immediately stops and abdominal pain appears, this is not very good, since there is a high probability that a spasm of the cervical canal has occurred and a hematometra
.
You must immediately contact your doctor
and inform him about this. He will invite you for an ultrasound and if the spasm is confirmed, they will quickly help you.
To prevent hematomas in the first days after curettage, you can take No-Spa 1 tablet 2-3 times a day.
In the postoperative period, you should be prescribed a short course of antibiotics
– this is necessary to prevent inflammatory complications.
The results of histological examination are usually ready 10 days after surgery, do not forget to pick them up and discuss them with your doctor.
In conclusion, I would like to note that curettage is one of the most frequent and most necessary minor operations in gynecology
. It is indispensable in the treatment and diagnosis of some gynecological diseases. Now this operation is very comfortable and can probably be called one of the most comfortable interventions available in gynecology, since you do not experience pain or discomfort. Of course, if you get to a careful gynecologist and anesthesiologist.
Rehabilitation after surgery
After the operation, the patient is sent to the ward on a gurney. A woman can get out of bed only 2 hours after completion of the procedure. When pain occurs, analgesics are prescribed. During the day, the woman needs to remain in the hospital under the supervision of doctors. To prevent the development of inflammation, antibacterial therapy is prescribed for 5 days.
After the operation, slight nagging pain may still appear in the lower abdomen for several days. Within two weeks - scanty discharge with blood. If they are very abundant or absent at all, then this is a serious reason for alarm and contact a gynecologist. Menstruation should begin 2-4 weeks after surgery. Sometimes after RDV the monthly cycle shifts to three months.
After the operation, visiting saunas and baths is prohibited, and you should temporarily abstain from sexual intercourse. During the first weeks, any physical activity or heavy lifting should be avoided. You can't use tampons. Hot baths can cause bleeding, so you should limit yourself to showering. You can return to sexual activity after at least two weeks, preferably after a month. The histology results will be known only after 15 days. Complications are very rare.
Recovery period
The woman is warned that bleeding will occur over several days (3-10). If they are absent, or there is pain, this may mean that complications have developed. After the operation, the doctor will definitely prescribe the woman antibacterial drugs to prevent inflammatory complications. During these days, while there is still bleeding, it is forbidden to take a hot bath.
Quite often, women after hysteroscopy with curettage experience pain in the lower abdomen, which is relieved with painkillers. It is recommended not to experience heavy physical activity for several weeks, including limiting sports activities. Do not lift heavy objects.
After the study, the woman should limit lifting weights
After the diagnostic and treatment procedure, you should not disturb the natural microflora of the vagina or use tampons. The administration of any intravaginal products should only be carried out as prescribed by a doctor.
Possible complications
After hysteroscopy with RDV, complications occur extremely rarely. The most common is uterine bleeding, when several pads are used in three hours. Other possible complications:
- Perforation of the uterine walls. During surgery, the cervical canal is usually injured. Serious pathologies change the structure of tissues, which become loose. Therefore, sharp instruments cause injury even with slight pressure.
- Endometritis is inflammation of the inner lining of the uterus. Appears due to infection and failure to treat with antiseptics. The first symptoms are severe sharp pain and high fever.
- Hematometra are blood clots in the canal that close the uterine opening. This provokes the development of an infectious process. This is accompanied by dizziness, high fever, and nausea.
- Asherman's syndrome appears after a frozen pregnancy or postpartum curettage. Reproductive abilities and the monthly cycle are disrupted. Adhesions form in the uterus.
However, with the addition of separate curettage of the hysteroscope, the operation becomes less traumatic and occurs without complications. The most common mild side effect is the appearance of bruises, but they disappear in just a few days.
Hysteroscopy with RDV allows you to identify diseases and neoplasms at an early stage. The procedure is much safer than simple scraping. This helps to make an accurate diagnosis and prescribe timely treatment.
- Pregnancy after hysteroscopy
- Laparoscopy is a new method of diagnosis and surgery
- Pregnancy after laparoscopy: when is conception possible?
- The test is positive, but the ultrasound does not show pregnancy
- Recovery after hysteroscopy of the uterus. Polyp removal.
Tests required before curettage
List of tests for planned curettage:
- complete blood count (CBC);
- general urinalysis (UCA);
- coagulogram;
- analysis for blood group and Rh factor;
- blood for syphilis, HIV, hepatitis;
- blood biochemistry (according to indications);
- smear for flora, oncocytology.
Instrumental research methods include:
- electrocardiography;
- fluorography;
- Ultrasound;
- hysteroscopy - performed before curettage to clarify the nature of the disease and localization of the formation, after - to control the thoroughness of tissue excision.
During emergency intervention, only the most necessary tests are performed, with which you can assess the patient’s condition as a whole:
- UAC;
- OAM;
- blood type and Rh factor;
- coagulogram;
- blood for sugar.
The planned operation is performed on an empty stomach; the hair in the perineum must first be shaved. You need to bring a robe, shirt, socks, a change of clean shoes, and pads. A few days before the procedure, you should stop douching, using vaginal pills and suppositories, and refuse sexual intercourse.