Accuracy of the method: can MRI make mistakes in diagnosis?
To obtain images, a device is used that scans the selected area in different projections. The device may not be able to distinguish small lesions unless a contrast agent is additionally used.
Sometimes errors are caused by the use of outdated models or failure to follow the rules of the study. Almost always, the images contain artifacts that are caused by the normal functioning of internal organs, movement during breathing, etc., but doctors are aware of this and take into account the presence of natural interference. The likelihood of device failure is minimized.
MRI is a tool. The images provide an opportunity to diagnose diseases after analyzing the changed tissues and the nature of the deviations. The decoding is carried out not by the device, but by the doctor, so the likelihood of detecting pathology depends on him, the reliability of the collected anamnesis and the results of other studies.
Indications for MRI and CT procedures
There are diseases for which it makes no significant difference what kind of research you undergo. Both one and the second device will be able to give an accurate result.
However, there are pathologies in which it is worth thinking about what is better - MRI or CT?
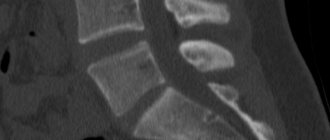
They are most often prescribed when there is a need to study in detail the soft tissues in the body, the nervous system, muscles, and joints. In such photographs, all pathologies will be clearly visible.
But the skeletal system, due to its low content of hydrogen protons, does not respond well to magnetic radiation, and the result may not be entirely accurate. In these cases, it is better to perform a computed tomography scan.
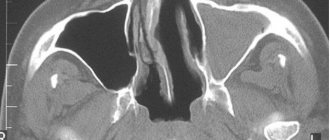
CT can also provide a more accurate picture when examining hollow organs, such as the stomach, intestines, and lungs.
If we talk about diseases, then MRI is indicated for:
Computed tomography is best performed to examine:
- Organs of the respiratory system.
- Kidney.
- Abdominal organs.
- Skeletal system.
- When diagnosing the exact location of injuries.
Thus, it becomes clear that the difference between MRI and CT lies in different points of application.
How often do errors occur?
Initially, erroneous results are obtained in 1-2% of cases. Most often, small focal changes cannot be detected on the images. As a result, the doctor concludes that there are no internal pathological injuries. Sometimes photographs show abnormalities that are not actually there. This is due to the appearance of artifacts - interference that arises as a result of magnetic susceptibility, movements and other factors.
In 34% of cases, an error occurs at the MRI decoding stage. Every third initial diagnosis turns out to be incorrect. Most often this is due to ambiguous interpretation of the results or insufficient qualifications of the doctor. The likelihood of an incorrect diagnosis after an MRI depends on a number of conditions. If a person has undergone a full examination and passed additional tests, the risk of receiving an error is reduced.
What is the likelihood of an erroneous diagnosis after a tomography?
MRI (magnetic resonance imaging) is a diagnostic method with high accuracy. As a result of the examination, the doctor receives images that show numerous sections of the organ being examined, directed in planes.
After completing the procedure using special equipment, all obtained images appear on the computer. Can MRI make mistakes in diagnosis? This depends on a number of factors.
Everything, from preparation for the procedure to the doctor’s conclusion, is directly related to an accurate diagnosis.
Why do diagnostic errors appear?
Incorrect diagnosis may be due to either a medical error or a violation of the procedure technology on the part of the specialist setting up the device or the patient. The likelihood of receiving unreliable images if the rules are followed is extremely low. This can happen when using outdated or broken equipment. Most often, patients in private clinics without a license encounter initially unreliable results.
Violation during research
During the scan, you are prohibited from moving. It is recommended to hold your breath if possible. This is due to the high accuracy of the images and the relatively small distance between projections. As a result, due to movements, the overall picture may turn out to be unreliable due to insufficient scanning of any layer or blurred images.
Contraindications include various neuroses, psychological disorders and childhood. Patients with such conditions involuntarily make movements during the examination. People in these categories can be admitted if absolutely necessary, but general anesthesia is recommended. Additionally, the study may not be informative in overweight patients (more than 110-120 kg). The standard device is not designed for high weight, so it is necessary to warn the doctor in advance.
Magnetic resonance diagnostics are incorrect if the specialist has configured the device incorrectly. If the mode or planes are selected incorrectly, the images become more difficult to decipher. The doctor may not detect focal changes if they are present. Often, at the interpretation stage, specialists are faced with incorrect definition of the center and the absence of some lobes in the image. The images must capture the entire organ under study and be symmetrical. To do this, staff must position the patient correctly.
Artifacts that may be mistakenly perceived as pathological lesions often arise from non-uniform magnetic susceptibility. The MRI may be incorrect if the patient does not remove jewelry. On the day of your visit to the clinic, it is recommended to wear clothing that does not contain metal inserts. It is necessary to warn the doctor if there are implants or foreign bodies in the internal organs. You should avoid using deodorant, talcum powder or lotions as they may cause darkening.
An error may occur at the stage of developing the image. Over-processing creates interference that creates additional shadow. If underdeveloped, the contrast of the image is too low. Failure to comply with the temperature conditions can lead to artifacts in various areas or throughout the image. After development, photographs should be stored in a dark, dry place as they may become damaged.
Incorrectly chosen method
In some cases, MRI either cannot indicate the cause of symptoms due to the specific characteristics of the radiation, or additional studies are required. This may be due to the absence of pathological changes in the tissues. MRI is more often used to examine blood vessels, joints and soft tissues. The procedure helps to assess the condition of the central nervous system, detect inflammation and identify tumors.
Due to its distinctive characteristics, the procedure may not be effective enough for some pathological processes. For example, for internal bleeding, injuries and examination of the chest cavity and genitourinary system, CT is preferred. This is due to the use of a different type of radiation.
In some cases, the use of a contrast agent is required. The technique should be used when cancer is suspected or to monitor the patient’s condition during treatment in the presence of tumors. The use of a contrast agent helps to identify relatively small formations, including metastases.
Insufficient qualification of a radiologist
Most often, errors are associated with incorrect interpretation of results. To obtain a correct MRI conclusion, a specialist must have knowledge of anatomy and pathology. The lesions are actually difficult to decipher. Doctors often mistake structural features, normal structures in a section, or artifacts for altered areas.
To identify a disease, a specialist must understand how pathological changes and the natural functioning of organs affect the image that the device displays. Noise in the images may occur due to the movement of blood vessels. Sometimes this is interpreted as the presence of tumors.
Additionally, to exclude errors, the doctor must obtain the results of other studies, collect anamnesis and take into account the totality of data. Third-party information helps distinguish similar pathological conditions.
How dangerous is computed tomography for the body?
Risks of CT include:
- allergic reaction to contrast agent;
- exposure to radioactive x-rays.
CT scans expose you to more radiation than conventional x-rays.
Frequent CT scans over a short period of time may increase the risk of developing cancer. However, the risk from a single scan is extremely low.
Some people are allergic to contrast dye. Most intravenous contrast agents contain iodine.
If the patient has a known allergy to this substance, administration of contrast may cause nausea, vomiting, sneezing, itching, or a rash.
If the use of contrast is absolutely necessary, your doctor may prescribe antihistamines or steroids before administering the contrast agent.
Asks: Marina367799
Female gender
Age: 37
Chronic diseases: not specified
Hello! For several years I have been bothered by a cough. At first I treated my throat. At the end of 2013 I had bronchitis in the fall of 2014. I fell ill with ARVI and with a strong cough two or three times there was blood in my saliva. Endless examinations began: I went through 5 ENT examinations - they found nothing serious except chronic pharyngitis and tonsillitis, took an X-ray of the lungs - they were normal, did a CT scan of the chest: “on a series of MSCTs, focal and infiltrative changes in the lungs are not detected. The pulmonary pattern is somewhat enhanced due to the vascular component. The lumen of the trachea, main, lobar and segmental bronchi on both sides is not narrowed, their course is not changed, the walls are not thickened or compacted. The roots of the lungs are structural and not expanded. The mediastinum is located centrally. The heart chambers are of normal size. The diaphragm is located normally, its contours are smooth and clear. The mediastinal lymph nodes are not enlarged. The axillary lymph nodes are not enlarged. The thoracic aorta is not changed. Pulmonary trunk dia. Up to 2.4 cm, right pulmonary artery up to 2.1 cm, left up to 2.0 cm. There is no free fluid in the pleural cavities. Bone destructive changes in the study area are not detected. » I did spiriography and allergy tests for domestic mites - they diagnosed mild bronchial asthma. For a while, I calmed down that everything was not so scary, I treated my asthma, but from time to time, more often in the evenings, I noticed wheezing and a slight dry cough when I exhaled strongly. But about a month ago I fell ill with ARVI and again with a strong dry cough I started bleeding from my throat (I decided that the blood vessels were bursting). ARVI quickly turned into bronchitis, purulent sputum began to leave, I took it for analysis. And they find atypical cells in it! I find out the result in a week, after treatment with antibiotics, I take the test again - the result is good. But I can’t get it out of my head where the atypical cells first appeared, why does blood appear when I cough? Can a CT scan result be wrong? Thank you in advance.
Is surgery advisable for my diagnosis or is alternative treatment possible? Evgeny Fedorovich. In August 2020, I underwent fluorography, which showed darkening in the second segment of the lung. Examination in May 2020. She was treated for pneumonia, a subsequent image showed the presence of the same darkening without change. The result of the first RCT on October 10, 2020: The mediastinum is located in a typical place, not enlarged in size, with clear contours, normal shape, without focal pathological formations. In the parenchyma of the S1-S2 segments of the upper lobe of the right lung, heterogeneous interstitial changes are determined due to polymorphic foci, ranging in size from 8.5 mm to 44.1 mm in diameter, against which areas of compaction like ground glass are visualized. In other segments, the parenchyma is without focal pathological formations, normal pneumatization. The architecture of the pulmonary and vascular pattern of the lungs is without any features. The lumen of the trachea and main bronchi is free, the walls are without pathological changes. The pulmonary sinuses are free, without pathological changes. The pulmonary sinuses are free, without pathological changes. The pleural layers are not thickened. Lymph nodes of the anterior mediastinum (sternal, prevascular and precordial) are not visualized. The lymph nodes of the posterior mediastinum are not enlarged. The lymph nodes of the central mediastinum are not enlarged. Repeated RCT January 9, 2020 gave the same result, the only difference is in size: in the first case from 8.5mm to 44.1mm. In diameter, in the second case from 9.6 mm to 44.4 mm in diameter. The result of a lung biopsy dated October 17: Tumor-like stenosis of the B2 upper lobe bronchus on the right, grade III (complete) due to obstruction of the lumen (with decay). Biopsy result dated October 20, 2020: Consolidation of the upper lobe of the right lung (atelectasis). Tumor-like stenosis (B2) of the upper lobe bronchus on the right, degree III, due to obstruction of the lumen, compression from the outside and infiltration of the mucous membrane (with decay). The tumor marker results are negative. Thank you in advance for your understanding
What to do if you doubt the result
If there is any doubt, the patient's further actions depend on a number of conditions. If the images were obtained recently, it is recommended to contact 1-2 other doctors. It is advisable to sign up for an individual consultation, because with remote communication, the specialist will not be able to examine the patient and correctly assess the state of health. Reviewing the images by multiple doctors will reduce the chance of misdiagnosis.
If the opinions of specialists do not coincide, it is recommended to undergo a re-examination. The probability of receiving an error at the stage of the procedure is lower than at the time of decoding, but it exists. The presence of several versions may be due to the presence of ambiguous interference or pathological foci in the images. Distinguishing artifacts from atypical tissue changes can be difficult. Some of the interference can be eliminated after a re-examination.
If the patient has already consulted a doctor before and a pathology has been identified, it is recommended to visit the same clinic to monitor the health status. When examined in another hospital, changes may not be detected due to the specific features of the device or incorrect settings.