Trophic (nutrition) disorders of cerebral structures are represented by a large group of pathological processes.
If we exclude variants with a chronic course, we can distinguish only two acute varieties, according to the classification:
- The first is a classic stroke. Acute malnutrition of the brain with parallel development of necrosis of neuronal clusters. This is the most dangerous type of violation.
Not heterogeneous (homogeneous) in nature, has several subspecies. Hemorrhagic (bleeding in the brain as a result of a ruptured vessel) and ischemic (tissue death due to insufficient blood supply).
It can also be primary, secondary, or localized in different parts of the brain.
They also differ in the extent and area of affected tissue. This disease alone deserves many scientific works.
- The second is a micro-stroke. There is no such diagnosis in the international classifier. We are talking about a transient or transient ischemic attack.
That is, a sharp significant decrease in the quality of brain nutrition but with no necrosis.
Therefore, this form is considered less dangerous: there is no tissue death, spontaneous regression of the disorder is observed even without medical assistance.
Thus, acute cerebrovascular accident, abbreviated as ACVA, is a disorder of insufficient speed and poor quality of blood flow in cerebral structures, provoking focal neurological symptoms and a reduction in certain functions of the central nervous system. There is a possibility of death.
Mechanism of formation and types of stroke
Acute circulatory disorders in the brain develop in several ways. Among the key ones, three can be named.
The first is atherosclerosis. The essence of the disorder is the narrowing or blockage of an artery located in the brain. In 95% of cases, the culprit is a cholesterol plaque.
Slightly less common is a blood clot that has broken away from the site of its own formation (usually the legs or arms, sometimes the heart).
Blocking the lumen leads to the inability of blood to move further or to a decrease in the efficiency of fluid tissue circulation. For the most part, this ends with a decrease in the quality of trophism (nutrition) of nerve fibers.
In the case of predominant blockage, especially if there are problems with the vessels, a rupture with the formation of a hematoma and massive bleeding cannot be avoided.
The condition is called hemorrhagic stroke, which also refers to an acute disorder of brain nutrition.
Atherosclerosis is also represented by narrowing (spasm) of the vessel. Usually the problem is observed in smokers, patients with diabetes, pregnant women, patients with congenital anomalies of the structure of the arteries, people who have suffered from inflammatory vascular diseases and others.
The second possibility is persistent, long-term hypertension. With a prolonged increase in pressure, the thickness of the walls of blood vessels increases, they lose elasticity, and the lumen narrows.
Hence the high probability of ischemia (cell death as a result of insufficient blood supply).
A spontaneous surge in pressure with the same outcome is also possible, and this option occurs in people without hypertension and generally without health problems. In case of inadequate physical activity, taking certain medications.
Finally, there is a third mechanism. It is associated with past inflammatory diseases (for example, vasculitis) affecting the choroid from the inside (intima or endothelium). Scarring and mechanical closure of the lumen of the tubular structure occurs.
Thus, despite the “cosmetic” differences, the essence is the same: disruption of blood flow, increased pressure in the vessel and further tissue death as a result of the impossibility of blood movement or rupture.
The etiology is identified to prevent an emergency.
A transient ischemic attack develops according to the same laws, but with it there is no rupture of blood vessels, and the death of neurons is not observed.
Therefore, these pathogenetic factors are milder in nature. Otherwise everything is identical.
The symptoms are similar, but the duration of the disorder is a maximum of a few hours, it goes away without a trace and does not leave a neurological deficit.
Death also does not occur, with one exception: involvement of the brain stem in the process.
Ischemic cerebral stroke
Ischemic stroke ranks first on the list of acute cerebral circulatory disorders (up to 85% of all cases). It often occurs during sleep and immediately after waking up.
The second name for the disease is cerebral infarction.
Causes
Ischemic stroke develops after intense physical activity, stress, or due to vascular atherosclerosis. The risk group for this disease includes patients with cardiovascular pathologies and diabetes mellitus.
A cerebral infarction occurs when the arteries are blocked (thrombosed) and the supply of oxygen to the cells of the organ is disrupted. Tissues deprived of nutrition die, forming a focus of pathology. The area of necrosis leads to permanent impairment of brain function. The disease is often preceded by a myocardial infarction suffered by the patient.
A thrombosed artery blocks oxygen supply to the brain, leading to ischemic stroke
Symptoms of cerebral infarction
Ischemic stroke is characterized by the appearance of the main symptoms during sleep. After a seizure, the patient may be conscious. Signs of a cerebral infarction:
- sharply increasing headache;
- paralysis of the muscles of the face, body and limbs (develops on the side opposite to the lesion);
- blurred vision and slow speech.
How to detect a stroke at home
At home, the patient's relatives can conduct tests for a possible stroke. Before the ambulance arrives, you need to ask the victim:
- show teeth or smile. In the presence of an ischemic stroke, a clear asymmetry of the lip line is visible in the patient. The corner of the mouth sags down on one side;
- repeat several words related in meaning. After a stroke, a person cannot pronounce phrases clearly. Speech changes, becomes unclear, the patient drawls out his words;
- Raise your arms at an angle of 90° and hold them in this position for 5 seconds. With ischemic brain damage, the patient drops one hand, unable to maintain the allotted time.
A checklist for identifying a stroke will help identify a person’s acute cerebrovascular accident before the ambulance arrives.
Home diagnostic measures should be carried out at the first suspicion of a stroke. The presence of one or more symptoms is a reason to immediately call an ambulance. It takes minutes to provide emergency care to a patient. Intensive therapy in the first few hours after an attack increases the chances of a full recovery.
Differential diagnosis
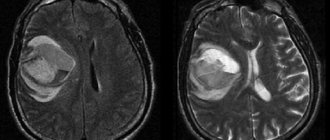
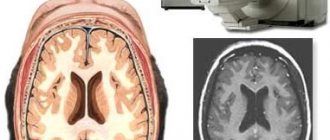
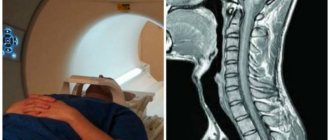
After hospitalization of a patient with suspected ischemic stroke, CT or MRI are prescribed. Modern techniques for visualizing brain lesions make it possible to clearly see the focus of the disease in the tissues and determine its type. In other words, to distinguish ischemic stroke from hemorrhagic or other intracranial pathology.
- Magnetic resonance imaging is a leading test in the differential diagnosis of strokes. The images clearly show the main signs characteristic of a cerebral infarction:
- tissue necrosis;
- edema;
- blockage of blood vessels.
- Computed tomography allows you to detect the presence of stroke and distinguish ischemia from hemorrhagic hemorrhage.
- Ultrasound with Dopplerography and duplex scanning is used for a complete examination of the condition of the patient’s carotid arteries. A study of cerebral blood flow makes it possible to clarify the diagnosis and prescribe better treatment for a patient with ischemic stroke.
Treatment of cerebral infarction
It is important to take emergency measures to provide medical care in the first 2–3 hours after the development of symptoms of a cerebral infarction, otherwise the tissue at the site of the lesion will die. Prescriptions must be made by an emergency doctor or resuscitator in a hospital.
- Intravenous administration of blood thinning drugs helps stop the development of paralysis (if used in the first three hours).
- Injections of drugs that reduce brain swelling and reduce intracranial pressure.
- Surgical intervention (stenting, endartectomy, angioplasty) prevents the risk of recurrent cerebral infarction by more than 50%. The operation is performed when the carotid artery is blocked.
The patient is in the hospital for 10 to 21 days. The dynamics of the disease are monitored using blood tests, CT, ultrasound or MRI.
With timely emergency assistance, a complete recovery of the patient is possible. If time is lost, doctors release the patient to home care after resuscitation and supportive measures.
Rehabilitation
After the patient is discharged from the hospital, it is important to treat the complications associated with the stroke:
- impaired motor function of muscles;
- speech and visual abnormalities;
- bedsores;
- pneumonia;
- thromboembolism of deep veins of the lower extremities, etc.
A patient after a stroke needs constant care and attention. With mild to moderate severity of the disease, it takes from several months to 1 year to restore lost functions (the ability to walk, talk, self-care skills). In severe cases, the patient remains bedridden or moves using a wheelchair.
It may take a long time to restore lost functions. As a rule, after a stroke, patients move in a wheelchair
The rehabilitation program is drawn up by a doctor. It includes:
- mandatory use of medications: antihypertensives, anticoagulants, cholesterol-lowering drugs (Piracetam, Capoten, Aspirin, etc.);
- feasible physical exercises (Feldenkrais exercises, exercise therapy);
- walks in the fresh air and simple work activities;
- therapeutic massage and physiotherapy (magnetic therapy, muscle stimulation with electrical impulses, applications of therapeutic mud and ozokerite, etc.)
Therapeutic exercise therapy in stroke rehabilitation - video
Nutritional Features
Patients who have suffered an ischemic stroke should refrain from drinking alcohol and smoking. Doctors recommend following several healthy eating rules during the rehabilitation period.
- Limit the amount of salt and sugar in dishes.
- Eat eggs, vegetable oil and fatty foods less often.
- Eliminate margarine from your diet and reduce your intake of flour foods.
- Try not to eat canned foods, pickles and marinades.
After a stroke, the body needs animal protein to restore the activity of the nervous system (chicken, lean beef). It should be steamed or boiled, then crushed in a blender and given to the patient in small portions. Fried foods are excluded from the menu forever. A person needs to drink up to 1.5 liters of fluid per day. It is recommended to give the patient water from a teaspoon.
Nutritionists recommend including the following foods in your diet:
- vegetables, fruits and dishes made from them;
- salads;
- cream soup;
- cottage cheese, kefir;
- dried apricots, raisins, prunes.
Prohibited products - gallery
Sauce Smoked products Sweets Bakery products Fatty dishes
Causes and risk factors
The moments were partially named. If we systematize all the possible ones, the following picture is created:
- Arterial hypertension. At the first stage, the likelihood of developing a stroke or transient ischemic attack is minimal. Then the risks increase. By stage 3 hypertension, when blood pressure is constantly high and the patient does not feel symptoms, the probability of a negative outcome is maximum and ranges from 15 to 25% during the year. Constantly.
- Atherosclerosis. Narrowing of the vessel or blockage of the structure by cholesterol plaque. Both options are dangerous. Requires urgent treatment.
- Endocrine diseases. Diabetes mellitus and under or overproduction of thyroid hormones are just some of the possible conditions that can trigger a stroke. Indirectly or directly.
- Osteochondrosis or hernia of the cervical spine. It provokes stenosis of the vertebral and basilar arteries, with disruption of the nutrition of the occipital lobe of the brain.
- Pathologies of the cardiovascular system. With low contractility of the myocardium, there is not enough blood to nourish the cerebral structures.
With a gradual increase in cardiac dysfunction, microstrokes often develop and only then full-fledged necrosis of nerve tissue.
Among the risk factors:
- Bad habits. Alcohol abuse, drug addiction, smoking.
- Physical activity is inadequate to the body's capabilities. It provokes excessive activity of the heart, and from a certain point the contractility decreases, and the organ becomes unable to provide for the brain. A common variant of deviation due to this reason is ischemic stroke. Hemorrhage is slightly less common.
- Stressful situations. One-time or permanent. They cause the production of hormones such as cortisol, adrenaline, followed by angiotensin and aldosterone. The substances artificially constrict blood vessels and cause secondary atherosclerosis.
- Poor nutrition, excessive consumption of animal fat.
- Lack of normal sleep.
- Presence of pulmonary diseases (if the respiratory system is affected).
- Taking certain medications: non-steroidal anti-inflammatory drugs, hormones, oral contraceptives, psychotropics (neuroleptics, antidepressants, tranquilizers).
Causes are assessed in the system to determine the likely outcome, diagnosis and treatment pathways for patients.
The basis of treatment is the elimination of the main provoking factor. Only by identifying the root cause is it possible to radically influence the situation and prevent a relapse.
Reasons for the development of the disease
There are a sufficient number of causes that can significantly affect the state of the cardiovascular system and cause various circulatory disorders. Conventionally, all reasons are divided into five groups:
- compression;
- traumatic;
- vasospastic;
- associated with the occurrence of tumors;
- occlusal.
Often, circulatory disorders occur in people with certain diseases, such as hypertension, diabetes, kidney failure, etc.
Conditions for the development of circulatory disorders, as a rule, are penetrating injuries, vascular disorders, aneurysms, and Raynaud's phenomenon.
Treatment of circulatory disorders directly depends on determining the cause with which it is directly related.
Signs of transient ischemic attack
General signs of stroke of a transient, transient nature are represented by classic manifestations of stroke, but differ in a number of ways:
- Insignificant in duration. The condition lasts from a couple of minutes to several hours.
- Complete spontaneous regression of symptoms. No medical intervention.
- No persistent neurological deficit after. The person returns to the “original position” the same as he was before.
Read more about the symptoms and treatment of transient ischemic attack here.
A stroke in itself is much more dangerous, because everything is exactly the opposite. Symptoms of acute cerebrovascular accident are divided into general and focal.
Let's sum it up
The difficult-to-understand abbreviation ACVA is the medical name for stroke, which is considered one of the most dangerous manifestations of cardiovascular problems for health and life. According to statistical data, stroke occupies the second place in mortality in the world, therefore every person who is concerned about their health should know about its manifestations, symptoms and prevention.
Despite the severity of treating the pathology, it has simple methods of prevention, even if a person is at risk for developing a stroke. The most important rule of prevention is to lead a healthy lifestyle, regularly undergo examinations in medical institutions, take timely measures to eliminate any negative manifestations of the body, and the likelihood of avoiding a diagnosis of stroke will increase several times.
Common stroke symptoms
The first are represented by nonspecific manifestations:
- Headache. Strong, unbearable. It is localized in the occipital region, crown, temples, and can cover the entire skull, spreading diffusely and radiating to the eyes and neck.
- Vertigo. Inability to navigate. The world is literally spinning, it’s impossible to even walk normally. Often a person takes a forced lying position.
- Nausea, vomiting. Short-term symptoms. Indomitable reflex gastric emptying almost never occurs. There is no relief after the act, because a false defense mechanism is triggered.
- Weakness, lethargy, drowsiness. Asthenic moments.
For a detailed description of stroke symptoms, read this article.
Focal signs
More specific and informative. Multiple areas of the brain may be affected.
Frontal lobe
Responsible for cognition. Creativity, thinking, behavior, everything is localized here.
Typical symptoms include:
- Marked decrease in intelligence, inhibition and decline in thinking productivity.
- Goofiness, inappropriate emotional reactions. Behavioral disorders may not be noticeable at first, because the patient is unable to demonstrate personal qualities. He is apathetic, mostly lies down and is silent.
- Regression. Induced infancy. Complete immaturity. Again, this refers to a behavioral disorder.
- Epileptic seizures. Heavy. Tonic-clonic. They can be repeated repeatedly, developing not into an attack, but into a status (a long course of paroxysms continuously or one after another for 30 minutes or more).
- Paralysis of the muscles opposite the localization of the lesion to the side.
- Aphasia. Inability to speak clearly.
Parietal lobe
Responsible for intellectual activity (partially), processing of tactile information (sensory component of human activity), and also the perception of smells.
- Inability to read, write, or perform simple arithmetic operations.
- Physical hallucinations. It seems to a person that someone is touching him, something is moving under the skin.
- There may be a lack of holistic perception of one's own body.
- There is agnosia, the inability to recognize an object, even the simplest one, known to everyone, by touch with eyes closed.
- There are complex complex hallucinations of the type of oneiric clouding of consciousness.
Temporal lobes
Responsible for auditory analysis, memory, verbal abilities.
- Deafness or hearing loss.
- Inability to understand speech in one's native language.
- Lack of speech, telegraph type of process. The patient expresses himself in abrupt words with formal logic intact.
- Epileptic seizures. This time they rarely turn into a full-fledged status with a continuous long-term course of the episode. Otherwise, the clinic corresponds to people’s ideas about a similar condition (seizure).
- Memory impairment. Anterograde, retrograde. Global and partial amnesia.
Occipital lobe
Responsible for visual analysis. Hence the corresponding symptoms: the simplest hallucinations such as luminous points and geometric figures, loss of areas of visibility, blindness (temporary) and other moments.
Limbic system and cerebellum
When it is affected, there is no sense of smell. Against the background of destruction of extrapyramidal structures (cerebellum), the inability to navigate in space, muscle weakness, lack of normal coordination of movements develops, and nystagmus is provoked (rapid spontaneous movement of the eyeballs to the left and right).
When the brain stem is involved in the pathological process, catastrophic consequences are possible: disturbances in heart rhythm and breathing, even stopping one or the other, critical jumps in body temperature. Even against the backdrop of a transient attack.
There is no fundamental difference between the individual forms of the disorder.
Deviation of the ischemic type is somewhat easier, because there is no additional negative factor. Namely, a blood clot, a hematoma, which compresses the tissue.
Lesions of the hemorrhagic type are more lethal; for comparison, the ratio of deaths in the first and second forms of stroke is 20 versus 43% for the small-focal type and 70/98% against the background of extensive destruction of nerve tissue.
Reasons for the genesis of the disease
ACVA, as a disease of the most complex level of danger, often develops against the background of pathologies existing in the body, to which medicine classifies the following processes:
- Hypertension, with rapid changes in blood pressure.
- Congenital or acquired pathologies of the cardiovascular system of the body.
- Atherosclerotic processes in large vessels.
- Inflammatory processes in the heart or the structure of blood vessels.
- Loss of vascular tone and elasticity.
- Thromboembolism.
- Blood diseases.
- Diabetes.
- Previously suffered a heart attack.
Medicine lists the following social and subjective circumstances as additional factors that can trigger the development of pathology in combination with the precedents described above:
- The age of the person. The natural aging process of the body affects absolutely all its areas, including blood vessels, which lose elasticity and firmness over time. People of retirement age are more prone to acute stroke, but recent precedents often affect younger people.
- Drinking alcoholic beverages, especially in excessive quantities, and smoking.
- Excess body weight, which entails or is a consequence of cardiovascular problems.
- Sedentary, inert lifestyle, low level of physical activity.
- Poor nutrition, which contributes to the development of atherosclerosis and thrombosis.
- Unfavorable environmental conditions.
- Regular presence of psycho-emotional stimuli against the background of a person’s low threshold of stress tolerance.
In a complex combination of pathological processes in the body and factors contributing to the development of stroke, the likelihood of the disease increasing several times.
First aid
It turns out immediately, at the pre-medical stage. The main thing to do is call an ambulance.
Then the algorithm is:
- Calm and reassure the patient. Fussiness will not lead to anything good.
- Place the victim on his back in a half-sitting position so that his head and torso are slightly elevated. A cushion made from scrap materials or several pillows will do.
- Provide fresh air flow. Open the window, window. This is important because it is necessary to correct hypoxia (oxygen starvation), which inevitably manifests itself during a stroke and even a transient ischemic attack.
- Loosen the collar and remove body jewelry. If there are any.
- Closely monitor the patient's condition. Assess the heart rate (based on the pulse on the carotid artery), pressure level, and the number of respiratory movements per minute.
- If you lose consciousness, turn your head to the side to prevent choking on vomit.
- If necessary, carry out resuscitation measures: cardiac massage (palm on the other, both on the middle of the sternum, do 80-100 energetic and rhythmic passes pressing the area 5-6 cm until the heart activity is restored).
Artificial respiration is done only if you have the skill, every 10-20 massage movements. If you don't have one, it's a waste of time.
Attention:
In no case should you put your head below the level of your body, give any medications, allow the patient to move, especially walk, take a bath, shower, eat or drink a lot.
For a detailed step-by-step algorithm for providing first aid for a stroke, read this article.
Diagnostics
It is carried out after the condition has stabilized. Acute cerebral circulatory disorders require a minimal examination: measuring blood pressure, heart rate, respiratory movements, and identifying the integrity of reflexes. Next they provide assistance.
Only after recovery does it make sense to evaluate the situation more carefully and look for the reasons.
The list of events is quite long:
- Oral questioning of the patient and collection of anamnesis.
- Daily monitoring using a programmable Holter device. It measures blood pressure and heart rate levels. Provides information about indicators over a 24-hour period.
- Electro- and echocardiography. To exclude a cardiac etiology of the problem.
- MRI of the brain. To identify the consequences of a violation.
- General blood test, biochemical (especially with detailing the lipid spectrum), for thyroid, pituitary, and adrenal hormones.
Other methods are also possible. The diagnosis of stroke is specified and established. Then it is important to carry out regular preventive examinations, as part of prevention and rehabilitation.
Symptoms of acute cerebrovascular accident
Before the onset of stroke, precursors may appear in the form of short-term neurological disorders. In 75% of cases, an ischemic episode occurs during sleep. Symptoms appear over several minutes or hours and may gradually increase. An increase in blood pressure is typical on the first day of the disease. Patients are concerned about the following complaints: headache (90%), weakness (75%) and/or numbness (70%) in one half of the body/limbs, decreased vision (30%), speech impairment (45%). 15% of patients may deny the presence of weakness/numbness in the limbs.
A neurological examination reveals a general cerebral syndrome, contralateral hemiplegia, hemianesthesia, homonymous hemianopsia, adversion of the head and concomitant deviation of the eyes, central paralysis of the face, tongue on the contralateral half of the lesion, motor-sensory aphasia, alexia, acalculia. Anosognosia, a disorder of the body diagram, is determined by damage to the non-dominant hemisphere.
Treatment
Conservative (medicinal) predominantly. Upon arrival at the hospital, the first stage begins. The following medications are mandatory:
- Thrombolytics. Streptokinase and others. To dissolve blood clots and normalize the flow of liquid tissue.
- Statins. Eliminate cholesterol deposits on the walls of blood vessels.
- Diuretics. Furosemide or more powerful osmotic ones. As part of the prevention of cerebral edema.
- Antiplatelet agents. Restores the rheological properties of blood. Fluidity. Aspirin Cardio, Heparin.
- When there is a critical drop in blood pressure, Epinephrine and Dopamine are used.
- Increased blood pressure levels are controlled by antihypertensive drugs. There are many options, so it makes no sense to give specific names.
Next, therapy with slightly milder drugs is prescribed. In addition to diuretics, anticoagulants, and drugs for normalizing blood pressure, the following are indicated:
- Cerebrovascular. Normalizes brain nutrition and blood flow.
- Nootropics. Glycine. To restore metabolic processes in nerve fibers.
It is possible to use other means, such as protectors that prevent the destruction of blood vessels (Anavenol) and others. At the discretion of specialists.
Operations are performed according to indications if the cause is a vascular anomaly (for example, an aneurysm), severe atherosclerosis, which cannot be corrected with drugs.
Lifestyle changes are mandatory: giving up smoking, alcohol, drugs, unauthorized taking of medications, full sleep (at least 7 hours per night), physical activity within the limits of what is reasonable and allowed (walking in the fresh air at a slow pace), limiting the amount of salt (7 grams per day). day or less), diet correction (refusal of animal fat, fried foods, fortification, treatment table No. 10 is suitable).
Treatment of acute cerebrovascular accident
- Maintaining vital functions of the body, antihypertensive drugs (at blood pressure 200/120 mm Hg), anticoagulants (the appropriateness of prescription is determined by the duration of the disease and concomitant pathology), antiplatelet agents, vasoactive drugs (Cavinton, Actovegin, Cinnarizine) , "Instenon"), neuroprotectors ("Cerebrolysin", "Ceraxon", "Piracetam", "Gliatilin", "Semax"), "Reopoliglyukin", "Trental", decongestants ("Lasix", "Mannitol").
- Passive exercise therapy, breathing exercises, speech therapy classes.
- Consider thrombolysis upon admission within 3–6 hours of illness.
- Rehabilitation activities.
- Secondary prevention.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Heparin (anticoagulant). Dosage regimen: IV or SC in the initial dose - IV (injection) 5000 IU, maintenance: continuous IV infusion - 1000–2000 IU/h (20000–40000 IU/day), pre-diluted in 1000 ml of isotonic NaCl solution; regular IV injections - 5000-10000 IU every 4-6 hours; s/c (deep) - 15,000–20,000 IU every 12 hours or 8,000–10,000 IU every 8 hours.
- Lasix (diuretic). Dosage regimen: intramuscularly or intravenously (slow stream) 20-60 mg 1-2 times a day, if necessary, the dose can be increased to 120 mg. The drug is administered for 7-10 days or more, and then the drug is taken orally.
- Piracetam (nootropic drug). Dosage regimen: administered intramuscularly or intravenously, starting from 2.0-4.0 g/day, quickly increasing the dose to 4-6 g/day. After the condition improves, the dose is reduced and switched to oral administration - 1.2-1.6 g / day. (0.4 g 3-4 times a day).
- Cavinton (a drug that improves cerebral circulation). Dosage regimen: intravenously 20-25 mg in 500 ml infusion solution. Within 2-3 days, the dose can be increased to no more than 1 mg/kg/day. The average course duration is 10-14 days. After completing the course of intravenous therapy, it is recommended to continue treatment with Cavinton tablets, 2 tablets 3 times a day.
- Trental (vasodilator, improves microcirculation). Dosage regimen: two intravenous infusions per day (morning and afternoon), at a dose of 200 mg (2 amps of 5 ml) or 300 mg (3 amps of 5 ml) in 250 ml or 500 ml of 0.9% solution sodium chloride or Ringer's solution.
Rehabilitation
It is carried out immediately after stabilization of the condition. It consists of systematically taking medications (already named), activity (physical therapy, exercises), massage, kinesitherapy (the same exercise therapy, but more variable, includes passive methods when movements are made with the help of another person). Also psychotherapy, restoration of emotional background.
Rehabilitation lasts from 6 months to a year. In some cases, even more. A transient attack does not require recovery for the most part.
Read about treatment after a stroke here, and the rehabilitation process is described in this article.