Ultrasound examination of the fetus or perinatal ultrasound diagnosis has become an absolutely integral part of obstetrics. Fetal ultrasound is a huge help in the complex work of obstetricians, but sometimes it is not entirely clear how to interpret some of its results.
One of these controversial issues in perinatology is the detection of a hyperechoic focus or inclusion in the left ventricle of the fetus. Such an unexpected find, and even in the heart of an unborn person, frightens the expectant mother. Let's talk about what a hyperechoic focus in the fetal heart is and whether it is dangerous.
Description of diagnosis
At the location of the point, compaction of the cardiac tissue is detected; it can be caused by:
- salt deposits;
- the presence of pathology in the chromosome set;
- the presence of an additional chord, which does not affect the full functioning of the heart.
If the reason that caused the appearance of a white dot in the cavity of the heart is a large amount of salts, then by the third trimester it disappears and does not have any consequences for the fetus. The same applies to the chord, it can cause heart murmurs up to a certain age (usually disappear at 2-3 years), or disappears before birth. In any case, if it is present, it is necessary to regularly examine the child with a cardiologist.
The only danger is a diagnosis found in combination with chromosomal abnormalities. In this case, myocardial compaction poses a danger to the child’s life.
A hyperechoic focus in the left ventricle of the fetal heart may indicate the presence of Down syndrome if pathological chromosomal markers were identified during a blood test in the pregnant woman.
Possible complications and consequences
Most often, the accessory chord in the left ventricle of a baby disappears by the time of birth, but can be present in the heart until 2-3 years of age, and can persist for life.
Reference! This condition does not pose a threat to the baby’s well-being, but you need to be aware of it and not ignore preventive visits to the cardiologist.
The local pediatrician should also be warned about the child’s health characteristics in order to exclude erroneous diagnoses when listening with a stethoscope.
At what stage can the fetal heartbeat be heard?
The formation of the heart occurs in the fourth week of pregnancy. Within a week, transvaginal ultrasound can detect myocardial contractions. An ultrasound examination with an abdominal sensor can be performed at the eighth week. If at this stage there are no contractile processes of the myocardium, then we can conclude that the pregnancy is fading.
After formation, the heart contracts at a frequency of 110-130 beats, then the number increases significantly to 170-190 (the peak occurs in the eighth week), and after that the fetal heart beats again decrease to 120-160 per minute and remain virtually unchanged until birth.
Listening to the heartbeat using a stethoscope is possible only from the twentieth week; this is only available to experienced doctors. You can listen to the baby’s heartbeat yourself as early as the thirtieth week.
Possibilities of fetal echocardiography in the first trimester of pregnancy (11-14 weeks)
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Introduction
The relevance of the topic of prenatal diagnosis of congenital heart defects (CHD) is clear to all doctors who are involved in prenatal diagnosis, neonatology, pediatrics, cardiology, and genetics. CHDs are one of the leading causes of perinatal mortality and are registered with a frequency of 4-13 per 1000 live births [1]. Due to the fact that preventive measures to prevent congenital heart disease are not sufficiently successful, their prenatal ultrasound diagnosis seems relevant and necessary.
Numerous studies by foreign and domestic colleagues have repeatedly formulated and studied various risk groups for the occurrence of congenital heart disease. This was done to potentially narrow the group of pregnant women eligible for echocardiography at a tertiary center. Among these risk groups were:
- Families with a child with congenital heart disease.
- Families with congenital heart disease in one or both spouses.
- Women suffering from diabetes, systemic connective tissue diseases, hypothyroidism.
- Pregnant women with teratogenic exposure in early pregnancy (herpes before the 6-7th week) [2].
However, in parallel, other scientists rejected these risk groups, because most congenital heart diseases occurred in fetuses and children whose mothers were not included in any of the proposed risk groups. The only reasonable criteria for the so-called selective selection were recognized as pregnant women who were at risk after screening in the first trimester and pregnant women with suspected congenital heart disease during ultrasound examination of the fetus [3].
It is undeniable that the optimal period of pregnancy for studying the fetal heart is 20-22 weeks, however, most lethal and clinically significant heart defects can be diagnosed at the end of the first trimester of pregnancy. Let us quote the words of the head of the Fetal Medicine Foundation, Kipras Nicolaides, expressed on the pages of the FMF website (www.fetalmedicine.com): “An ultrasound specialist should assure most parents from the 12th week of pregnancy that their child does not have major congenital heart defects. In the case of large congenital heart defects, early detection can lead to a correct diagnosis or at least raise suspicion for ultrasound monitoring.”
The main goal of prenatal diagnosis has been formulated by prenatal diagnostic specialists around the world - to provide women with the maximum possible information about the defect as early as possible. We must give the woman and the family as a whole the right to decide on prolonging pregnancy with gross malformations in the fetus [4].
Every year, an increasing number of publications are devoted to the diagnosis of congenital heart disease in the early stages - in the first trimester of pregnancy [5-8]. Almost none of the issues of the ISUOG journal (Ultrasound In Obstetrics and Gynecology, or the “white” journal, as experts call it) ignores the topic of early diagnosis of congenital malformations.
The most famous website in the world of prenatal diagnostics, www.thefetus.net (Philippe Jeanty, USA), has already published more than 30 cases of congenital heart disease in the first trimester of pregnancy. However, in Russian periodicals there are only a few works on this topic. All of them belong to the “pen” of prenatal diagnostic specialists of the Russian Association of Ultrasound Diagnostics in Perinatology and Gynecology, although for many specialists, both before and now, examination of the fetal heart at 11-14 weeks consists only of ascertaining the number of heartbeats.
The purpose of echocardiography in the first trimester of pregnancy is to identify fatal and clinically significant congenital heart disease. This study does not aim to identify stenoses and hypoplasias of the outflow tracts, diagnose minor septal defects, pathologies of the aortic arch and ductus arteriosus. Many of these defects are not only technically impossible to suspect in the first trimester, they manifest themselves after the 30th week of pregnancy, i.e. their diagnosis is the prerogative of research in the third trimester.
The accuracy of prenatal diagnosis of congenital heart disease at all stages of pregnancy varies widely. The reasons for this may be different experience of specialists, obesity of the pregnant woman, frequency of ultrasound transducers used and class of ultrasound machine, previous abdominal surgeries, gestational age, amount of amniotic fluid and fetal position. However, we note that many of these factors lose their relevance precisely when transvaginal echocardiography is performed in the first trimester of pregnancy. Timely diagnosis of congenital heart disease makes it possible to identify high-risk fetuses based on genetic syndromes, which is important during prenatal counseling and has a significant impact on obstetric tactics.
results
From 2006 to 2011, 125 congenital heart diseases were detected prenatally in the first trimester of pregnancy. Of these, 68 (55%) CHDs were combined with various chromosomal anomalies (CA) of the fetus, 30 (24%) were part of various multiple congenital malformations (MCDM), 27 (21%) CHDs were isolated.
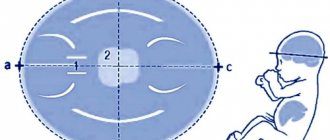
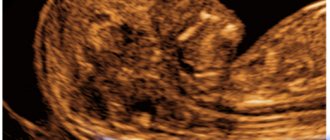
Echocardiography examined a four-chamber section of the fetal heart (Fig. 1) and a section through three vessels (Fig. 2). Ultrasound was performed with a transabdominal sensor; only when necessary (difficult visualization) was an intracavitary sensor used. A four-chamber section of the fetal heart during ultrasound scanning with a transabdominal sensor was visualized in 85% of cases, a section through the vessels - in 73%, when using a transvaginal sensor, these figures increased significantly to 100 and 91%, respectively. Optimization of prenatal diagnosis of congenital heart disease can be achieved through strict adherence to basic methodological rules. When assessing a four-chamber section of the fetus, it is necessary to evaluate the normal location of the fetal heart, excluding its ectopia (Fig. 3), the position of the axis of the fetal heart, which does not present any difficulties, the normal proportions and sizes of the chambers of the heart, the movement of the atrioventricular valve leaflets should be free, the septal leaflet of the tricuspid the valve should be located closer to the apex of the heart (Fig. 4). When assessing a section through three vessels, it is necessary to evaluate the relative position of the vessels and their diameter.
Rice. 1.
Pregnancy 12 weeks. Four-chamber section of the fetal heart. The chambers of the heart are clearly visible.
Rice. 2.
Pregnancy 12 weeks. Section through three vessels. The aorta and pulmonary trunk are visualized. The vessels are located in one line and have normal sizes.
Rice. 3.
Pregnancy 8 weeks. Ectopia of the heart. The heart is located outside the chest cavity.
The case was published on the website www.thefetus.net.
Rice. 4.
Pregnancy 13 weeks. Four-chamber section of the fetal heart. The chambers of the heart are clearly visible. Position of atrioventricular valves.
Advanced echocardiography involves the use of additional modes and sections - a section through the aortic arch (Fig. 5), a section through the outflow tract of the left ventricle (Fig. 6), a CD mode (Fig. 7), pulse Doppler, STIC technology (Fig. 8-11 ). This examination is carried out when abnormal screening projections of the fetal heart are detected, markers of CA [widening of the thickness of the nuchal space - TVP, hypoplasia/absence of the nasal bone (Fig. 12, 13), regurgitation in the ductus venosus (Fig. 14), tricuspid regurgitation (Fig. 15 )] and/or congenital malformations of the fetus.
Rice. 5.
Pregnancy 13 weeks. Section through the aortic arch. Three brachiocephalic vessels extending from the arch are clearly visible.
Rice. 6.
Pregnancy 12 weeks. Tetralogy of Fallot. Color flow mode. Section through the left ventricular outflow tract. The “equestrian aorta” is visible, sitting above the VSD. The case was published on the website www.thefetus.net.
Rice. 7.
Pregnancy 13 weeks. Double exit of vessels from the right ventricle. Color flow mode. Parallel exit of vessels from the right ventricle.
Rice. 8.
Pregnancy 12 weeks. Atrioventricular communication (AVC) in Down syndrome. STIC mode.
Rice. 9.
Pregnancy 12 weeks. Tetralogy of Fallot. STIC mode. The “horsewoman” aorta sits above the VSD. The case was published on the website www.thefetus.net.
Rice. 10.
Pregnancy 13 weeks. Transposition of the great vessels. STIC mode. A parallel course of efferent vessels is visible, the upper of which leaves the left ventricle and divides into a bifurcation (pulmonary artery).
Rice. eleven.
Pregnancy 12 weeks. Common arterial trunk. STIC mode. A single efferent vessel of two ventricles is visible.
Rice. 12.
Pregnancy 11.4 weeks. Multiple markers of CA. Patau syndrome (trisomy 13). Increased TVP, abnormal profile with hypoplasia of the nasal bone, protuberance on the upper jaw (a sign of a cleft face), polydactyly. The fetus was diagnosed with hypoplasia of the left heart.
Rice. 13.
Pregnancy 12 weeks. Multiple markers of CA. Down syndrome (trisomy 21). Increased TVP, abnormal profile with nasal bone hypoplasia. AVC was detected in the fetus.
Rice. 14.
Pregnancy 12 weeks. Reverse blood flow in the ductus venosus in a fetus with heterotaxy.
Rice. 15.
Pregnancy 12 weeks. Tricuspid regurgitation in a fetus with a common truncus arteriosus.
The nosology of the congenital heart diseases we identified was as follows:
- hypoplastic left heart syndrome (HLHS) - 29 cases (Fig. 16);
- atrioventricular communication (AVC) - 23 (Fig. 17, 18);
- ventricular septal defect (VSD) - 19 (Fig. 19);
- pathology of the great vessels - 19 (of which transposition - 3, double origin of vessels from the right ventricle - 2, tetralogy of Fallot - 5, common truncus arteriosus - 9);
- pathology of the right heart (pathology of the tricuspid valve) - 3;
- heterotaxy syndrome - 6;
- single ventricle - 4;
- ectopia of the heart - 7;
- combined forms of congenital heart disease occurred in 15 cases.
Rice. 16.
Pregnancy 13 weeks. Hypoplastic left heart syndrome in a fetus with Turner syndrome (45X). Single flow through the tricuspid valve. Shunting of blood into the hypoplastic left ventricle through the VSD.
Rice. 17.
Pregnancy 11.4 weeks. Four-chamber section of the heart. Single atrioventricular valve. There is no “cross” of the normal relationship between the atrioventricular valves and the heart septa.
Rice. 18.
Pregnancy 11.4 weeks. Four-chamber section of the heart. Color flow mode. Single atrioventricular valve.
Rice. 19.
Pregnancy 12 weeks. Color flow mode. Extensive VSD in a fetus with Edwards syndrome (trisomy 18).
When karyotyping fetuses with a prenatal diagnosis of congenital heart disease at 11-14 weeks, 68 chromosomal abnormalities were diagnosed:
- trisomy 21 (Down syndrome) was detected in 23 (34%) cases,
- trisomy 18 (Edwards syndrome) - in 19 (28%);
- trisomy 13 (Patau syndrome) - in 7 (10%);
- monosomy X (Turner syndrome) - in 6 (9%);
- triploidy - in 8 (12%);
- other chromosomal imbalances - in 5 (7%).
It should be especially noted that in 8 cases of detected CA, the indication for karyotyping was the identification of congenital heart disease. These fetuses had normal values for both TVP and nasal bone length.
In case of CA, the identified congenital heart disease according to nosology had the following features: in the majority of fetuses with Down syndrome, AVK and VSD were diagnosed; with Patau syndrome - GLOS and VSD; with Edwards syndrome - VSD, tetralogy of Fallot and OSA; with Turner syndrome - GLOS and aortic pathology - coarctation of the aorta in a typical place (Fig. 20).
Rice. 20.
Pregnancy 12 weeks. Section through the aortic arch. Color flow mode. Narrowing of the aorta in a “typical” location in a fetus with Turner syndrome (45X).
It is necessary to separately consider the issue of verification of ultrasound diagnosis. All pregnancies with isolated congenital heart disease in the first trimester were prolonged until the second trimester, when 100% morphological verification of the diagnosis is possible. In modern conditions, verification of diagnoses after termination of pregnancy in the first trimester is a rather significant problem. However, with specialized training of specialist morphologists, verification of congenital heart disease is also possible during termination of pregnancy in the first trimester (Fig. 21, 22). This undoubtedly depends on the quality of the material obtained, the qualifications of the morphologist and the special equipment required in some cases, as well as on the general methodological approaches to anatomical and morphological diagnosis, regardless of gestational age.
Rice. 21.
Pregnancy 13 weeks. Increased TVP in a fetus with hypoplasia of the left heart.
Rice. 22.
The same fruit. Morphological examination - hypoplasia of the ascending aorta and cystic cavities (marked by arrows).
Conclusion
From the above, the following conclusions can be drawn.
The fetal heart should be assessed in all pregnant women during a screening examination in the first trimester (11-14 weeks). Since the modern concept of the development of prenatal diagnostics within the framework of the “pilot” project of the Ministry of Health of the Russian Federation implies a screening examination in the first trimester by an expert doctor, it is he who should evaluate the fetal heart and suspect congenital heart disease at the end of the first trimester of pregnancy.
To exclude lethal and clinically significant cardiac pathology in the first trimester, it is necessary to evaluate the four-chamber projection of the fetal heart and the section through three vessels.
Extended echocardiography should be performed if abnormal screening projections of the fetal heart, markers of CA and/or fetal congenital malformation are detected.
If congenital heart disease is detected in the first trimester, fetal karyotyping is indicated.
Literature
- Office for National Statistics. Mortality statistics. Childhood, Infancy and Perinatal. Series DH3. Stationary Office: London, 2007; 40.
- Novikova I.V., Pribushenya O.V., Rumyantseva N.V. Formation of risk groups for prenatal diagnosis of congenital heart defects. Instructions for use. Minsk, 2004.
- Carvalho JS, Moscoso G, Tekay A et al. Clinical impact of first and early second trimester fetal echocardiography on high risk pregnancies. Heart. 2004; 90: 921-926.
- Becker R., Wegner R.-D. Detailed screening for fetal anomalies and cardiac defects at the 11-13 week scan. Ultrasound Obstet Gynecol 2006; 27; 613-618.
- Allan LD, Sharland GK, Milburn A. et al. Prospective diagnosis of 1,006 consecutive cases of congenital heart disease in the fetus. J Am Coll Cardiol 1994; 23: 1452-1458.
- Huggon IC, Ghi T, Cook AC et al. Fetal cardiac abnor-malities identified prior to 14 weeks' gestation. Ultrasound. Obstet. Gynecol. 2011; 20: 22-29.
- Persico N., Moratalla J., Lombardi CM et al. Fetal echocardiography at 11-13 weeks by transabdominal high-frequency ultrasound Ultrasound Obstet. Gynecol. 2011; 37: 296-301
- Allan LD Echocardiographic detection of congenitalheart disease in the fetus: present and future. Br. Heart. J. 1995; 74: 103-106.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
GEF Diagnostics
Golf ball syndrome is detected by ultrasound. After this, it is advisable to visit an additional 3D ultrasound; the attending physician may also refer the pregnant woman for fetal echocardioscopy. Most often this study is prescribed:
- pregnant women over 35 years of age;
- if the mother had infectious diseases in the early stages;
- if the pregnant woman (or relatives) has heart pathologies or diabetes mellitus;
- after a routine ultrasound reveals pathologies in the heart area;
- when the development of the fetus and its size are delayed;
- when markers indicating chromosomal abnormalities are detected.
A hyperechoic focus in the left ventricle of the fetal heart can be examined using echocardioscopy at 18-28 weeks, after which it will not be possible to conduct a full examination, since the size of the child will be too large to qualitatively examine the size and condition of his heart.
When is the examination carried out?
A hyperechoic focus can be detected by ultrasound, which may result in a 3D ultrasound or fetal echocardioscopy. The reason for ordering an examination may be:
- age of the expectant mother;
- infectious diseases suffered by a pregnant woman in the first trimester;
- diabetes mellitus or cardiac pathology in the mother or close relatives;
- previously identified heart problems in the fetus;
- developmental delay of the child (assessed by ultrasound);
- detection of markers of chromosomal diseases.
“Golf ball syndrome” can be easily detected by echocardioscopy if the gestational age exceeds 18 weeks, but has not reached 28 weeks. Later, it will not be possible to fully examine the baby’s heart, because the older child partially blocks the view.
Normal indicators during echocardioscopy
During the examination, all cavities of the heart are measured. Normally, these indicators should be within the limits:
- length of the right ventricle – 0.5-1.75 cm;
- width of the right ventricle – 0.4-1.1 cm;
- length of the left ventricle – 0.9-1.8 cm;
- left ventricular width – 0.44-0.89 cm;
- the ratio of the width of the left ventricle to the right is 0.45-0.9 cm;
- aortic mouth – 0.3-0.52 cm;
- the mouth of the pulmonary artery – 0.3-0.5 cm;
- mitral orifice – 0.35-0.6 cm;
- tricuspid foramen – 0.3-0.63 cm;
- number of heart contractions – 140-160 beats/minute.
The size of the fetal heart has its own indicators and differs significantly from the size of an adult, since all organs correspond to the size of the body. Heart pathology is always detected during such an examination, so you should not worry about the unprofessionalism of the uzist if the diagnosis is not confirmed or the doctor says that this does not pose a threat to the child.
What to do when identifying a GEF
GEF in the fetal heart involves the doctor prescribing additional routine examinations. These include:
- Ultrasound of the child’s heart with Doppler sonography;
- CTG (cardiotocography);
- 3D or 4D ultrasound.
If the diagnostic methods performed do not refute the presence of heart pathologies (that is, when there are pathological markers in the blood and these signs are confirmed by ultrasound), it is recommended to visit a geneticist.
Such a study is a very serious step, as it carries a great danger of miscarriage or fading of the pregnancy. Therefore, collecting cord blood or amniotic fluid is necessary only in the most extreme cases.
The heart pathology may be insignificant, then the geneticist will not refer you for such a dangerous diagnosis. However, when confirming the diagnosis using a volumetric ultrasound, it is better to consult with a professional about the danger of GEF for the baby’s life.
Hyperechoic focus in the left ventricle of the fetal heart: causes
The appearance of an echogenic focus in the child’s heart may be a consequence of mineralization of the vessels of the heart muscle, an individual feature of the heart (in which an additional septum in the heart is detected in the form of a small chord) or chromosomal pathologies, in particular Down syndrome.
The fetus develops very quickly over the weeks and its body and vital body systems improve even more. That is why it is necessary to regularly monitor the condition of the fetus, which will allow you to detect possible developmental problems in time or prevent them before the first symptoms appear.
If pathological chromosomal markers are present in the mother's blood, the presence of developmental abnormalities in the child is finally confirmed. In this case, parents must decide whether additional examinations or termination of pregnancy are necessary.
Consequences of the diagnosis for the child
Normally, the extra chord of the left ventricle in a child disappears at the end of the third trimester, but it can also remain in the heart all his life without posing a threat to health. You need to know about this and, if necessary, inform your pediatrician, since when listening there is a possibility of making an incorrect diagnosis due to the presence of a heart murmur.
It is also recommended to register with a pediatric cardiologist and be regularly examined for pathology. As a rule, by the age of three, any signs of inclusion in the heart muscle disappear in the child, then the doctor makes a conclusion about the absolute health of the child.
Should I worry about this diagnosis?
As a rule, a hyperechoic focus in the left ventricle of the fetal heart does not pose a danger to the child. After birth and a routine examination by a doctor, no deviations from the norm are detected in children; only minor noises are possible in the presence of an additional chord.
When the child reaches the age of 2-3 months, for greater peace of mind for the parents, an ultrasound of the heart can be done, which will detail all the sizes of the cavities and valve openings, the number of additional chords and the general condition of the cardiovascular system. In conclusion, a diagnosis will be written about the health of the heart and full compliance with age characteristics (usually, before the age of one year, children are diagnosed with an open foramen ovale).
Only in a small percentage of cases, an additional chord of the left ventricle in a child can lead to heart disease or other pathologies. But for this, the mere presence of “golf ball” syndrome is not enough; precise confirmation of the danger is necessary through sampling of amniotic fluid or blood from the umbilical cord and the presence, after diagnosing the blood, of pathological markers indicating the presence of chromosomal abnormalities in the fetus.
Are the worries justified?
Despite the fact that doctors advise not to worry ahead of time, many pregnant women are unable to cope with their emotions. As a rule, even with such a minor feature, the heart beats normally, without causing any discomfort to the child.
In the presence of a hyperechoic focus of the left ventricle of the fetal heart after the birth of a child, slight heart murmurs are detected, which are created by the peculiarity of the myocardial structure.
When the child reaches 2-3 months of age, an ultrasound diagnosis of the heart is prescribed, after which a conclusion is issued with a detailed description of the structures of the heart, its function, and size. Rarely, such a diagnosis may reveal an oval window - a small hole between the atria. As a rule, such a feature is closed within a year. If for some reason this does not happen, then detailed studies are prescribed and a decision is made on appropriate treatment.