Ultrasound of the scrotum
Ultrasound of the scrotum
is a widely used method for diagnosing various urological and other diseases. Used by urologists and other specialists when it is necessary to confirm or refute the presence of pathologies of various origins. The essence of this examination procedure is the ability of ultra-high-frequency sound waves to penetrate through body tissues and be reflected from them. This allows you to see and analyze the internal structures in the scrotum area, the condition of tissues, organs and structures, the vascular bed and local blood flow (using the Doppler mode), as well as identify the development of various diseases and pathological processes.
This diagnostic method is a non-invasive and safe procedure. Provides accurate visualization of the studied structures in the scrotum area and is highly informative compared to other research methods.
Regular examination using ultrasound allows us to identify the early stages of various diseases (including the development of malignant tumors), which in turn ensures an early start of treatment, prevents the development of complications and promotes cure.
Ultrasound of the prostate gland
Ultrasound of the prostate gland can be performed abdominally and transrectally. Transrectal examination is performed through the rectum. For this, a sensor is used whose dimensions do not exceed 2 cm. Therefore, the procedure does not cause severe pain or discomfort. During an abdominal ultrasound, the prostate gland is examined through the anterior abdominal wall.
Before examining the prostate gland using transrectal ultrasound, you need to do an enema. The patient must undergo this procedure 2 hours before the start of the examination. Before an abdominal examination, the patient should drink 1-1.5 liters of fluid approximately 1 hour before the procedure to keep the bladder full.
The transrectal method has an advantage over the abdominal one. When the sensor is inserted through the rectum, the prostate gland is much better visible on ultrasound, so the diagnosis will most likely be more accurate.
During an ultrasound of the prostate, its volume is studied (normally it should be 20-25 cm); width (in normal condition – 25-40 mm); thickness (1.7-2 mm); weight (20-25 grams); length (23-35 mm). An increase in the weight of the prostate, detected during an ultrasound, indicates that an inflammatory process is taking place in the gland. In addition, the shape (it should be similar to a chestnut), structure, contours and ducts are studied.
The cause of inflammation of the gland can be past infectious diseases (sore throat, pneumonia, carious teeth, and so on). Inflammation can be introduced into the prostate through sexual intercourse. Ultrasound can show the presence of abnormal processes. Their nature needs to be clarified using additional tests.
Ultrasound also does not have a negative effect on the prostate. There are practically no contraindications to such an examination (the exception is transrectal examination, which is not performed for hemorrhoids and anal fissures).
When is an ultrasound of the scrotum prescribed?
Ultrasound examination of the scrotum is an indicative research method. Due to the location of this area and its anatomical structure, ultrasound of the scrotum is often the only method with no alternative. However, it is often prescribed as part of a comprehensive examination, including laboratory tests. Sometimes the information obtained through examination of the scrotal organs is decisive in detecting diseases and making a diagnosis.
There are indications for which specialists refer the patient for this examination:
- male infertility;
- detection of an unnatural formation in this area upon palpation;
- erectile disfunction;
- swelling of the scrotum and/or pain in this area;
- the appearance of signs of inflammatory processes in the area of the testicles and scrotum in men (inflammation of the testicle - orchitis, inflammation of the epididymis - epididymitis, the inflammatory process affects the testicle and epididymis - orchiepididymitis);
- injuries to the pelvis or scrotal organs;
- presence of hemorrhages, hematomas;
- signs of slowing or accelerating the process of puberty in boys;
- deviations in spermogram;
- varicocele;
- enlargement of one or both testicles with sagging scrotum;
- enlargement of local lymph nodes;
- non-standard location of the testicles;
- endocrine diseases;
- for diagnosing inguinal hernias entering the scrotum;
- to monitor the condition of organs after surgical interventions;
- for monitoring and analysis of ongoing treatment measures;
- and etc.
#!UZIseredina!#
How are the results obtained interpreted?
The diagnostic standards are as follows: male testicles have a clearly defined contour and elastic consistency.
The surface of each of them is smooth, but the internal structure has a granular structure.
A characteristic age-related feature is a change in the sound permeability or density of the testicles. In boys who have not reached puberty, the density of the testicular structure is higher than in mature men.
It is advisable to check the testicles in men with a lack of testosterone, since subsequently this deficiency can significantly affect the course of metabolic and recovery processes.
Decoding will help determine:
- Cryptorchidism. A fairly common pathology, occurring mainly in boys of early childhood. Characterized by undescended testicles into the scrotum. Since this movement of testicles from the abdominal cavity is determined phylogenetically (for normal sperm formation, an optimal temperature of about 30 ° C is required, and a constant temperature of 37-38 ° C is maintained in the abdominal cavity), it is extremely important to identify this condition in the early stages of its development. An ultrasound cannot determine their presence in the scrotum, or a testicle with a short spermatic cord is detected, which indicates incomplete descent. The testicles are usually smaller than normal and there is no grain in the image.
- Tumors. Oncological processes of the testicles are rare, but can lead to serious consequences and metastasis. A tumor on ultrasound of the testicles is an irregularly shaped formation with an unclear structure, loss of granularity, and distortion of the surface. In parallel, there may be a significant decrease or increase in testosterone levels.
- Calcifications and cysts. They are detected in the case of age-related dystrophic changes and metabolic disorders (calcifications) or in early childhood (congenital cysts). Ultrasound of the testicles reveals a round formation in the testicular tissue, cavitary or complete, with clear contours and a density different from the testicular tissue.
- Inflammatory processes develop in the testicles most often either as a result of injury, or through hematogenous or lymphogenous transfer. During the procedure, it is possible to determine the swelling of the testicular membranes, their pain when touched by the sensor, and an increase in general temperature.
All these conditions require a high level of training of diagnostic specialists, since competent interpretation of the results obtained contributes to the correct diagnosis and determination of a further plan of action and treatment.
How is the procedure done?
Before the examination, the patient needs to be aware of how an ultrasound of the scrotum is performed. The examination is carried out in an ultrasound diagnostic room using a high-frequency sensor. The patient is asked to strip naked in the lower half of the body. Next, the person lies in a horizontal position on the couch on his side or back (for ease of diagnosis). After this, a special gel is applied to the skin in the area of the scrotum and testicles, which does not cause allergic reactions, in order to improve the sliding of the ultrasound sensor over the surface and ensure the necessary skin-sensor contact. Subsequently, the specialist passes the sensor over the required area, and through the action of ultra-high frequency sound waves and the operation of the ultrasound machine, the information is displayed on the monitor in real time.
The duration of the diagnosis varies from 15 to 20 minutes, however, if the doctor detects some pathologies, the procedure may be extended to 30-40 minutes.
After the examination is completed, the patient is given a conclusion and referred to the attending physician for a more complete analysis of the information received and individual selection of treatment (if necessary).
Ultrasound of the scrotum with Dopplerography
Ultrasound of the scrotum with Doppler ultrasound uses the Doppler effect. Thanks to the special mode of the ultrasound device, it becomes possible to determine the state of local blood flow, as well as superficial and deep vessels, pathological narrowings or expansions (aneurysms), blood clots, emboli and thromboemboluses, as well as atherosclerotic plaques that create an obstacle to normal physiological blood flow.
Dopplerography and its features
Ultrasound of the scrotum with Doppler is performed according to the same scheme. During the procedure, special sensors are used that record information about blood flow. Using Doppler sonography, the doctor can assess the quality and intensity of blood supply. This procedure is prescribed to patients with suspected testicular torsion, varicose veins of the scrotum, as well as a number of other pathologies associated with disruption of the structure or function of blood vessels.
Decoding the results
Both the ultrasound specialist and the specialist who referred the patient for diagnosis are involved in analyzing and deciphering the information received. The results will not take long to arrive and can play a decisive role in making a diagnosis.
What diseases can a scrotal ultrasound detect?
Diseases detected through ultrasound diagnostics of the scrotum include:
- male infertility of various etiologies;
- adnexal cyst;
- benign and malignant tumors of the appendages and testicles;
- abscesses in this area;
- inflammatory processes (epididymitis, orchitis, etc.);
- closed injuries;
- varicocele;
- hydrocele (dropsy of the testicle);
- the presence of calcifications;
- hypogonadism in children;
- and etc.
Operating principle of an ultrasound machine
The essence of its work is the formation of ultrasonic waves. The device's sensor contains a crystal. When an electric charge is passed through it, a piezoelectric effect develops, resulting in the formation of an ultrasonic wave. Using a sensor, it is directed to internal tissues and organs. Some of them have good permeability to ultrasonic waves, while others do not conduct it and reflect back.
The reflected wave is received by a sensor, which converts it into an image visible on a computer screen. The doctor determines visible changes, compares them with normal indicators and criteria and makes a preliminary diagnosis (describes the picture he sees and makes assumptions about the patient’s condition).
In what areas has this technique found its application?
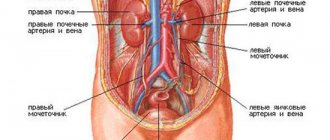
For the most part, ultrasound is used in those areas of medicine where it is necessary to visualize the internal environment of the body and determine the presence of cavity or liquid formations in it. That is why ultrasound is used to study the organs of the gastrointestinal tract, musculoskeletal (in children) and genitourinary systems. Ultrasound is especially widely used in urology and andrology. This study is necessary for diagnosing diseases of the kidneys, urinary system and genital organs.
This study is excellent for determining the condition of the testicles in men.
The procedure has become famous due to the instant receipt of research results and their prompt interpretation. With such a study, in most cases it is possible to determine the condition of the male gonads and identify the existing pathology.
Ultrasound of the bladder
An ultrasound of the bladder is performed if the patient is concerned about:
- pain in the lower abdomen;
- presence of blood in semen;
- infertility;
- difficulty, pain, stinging during urination;
- frequent urination (with a small amount of urine).
Before the ultrasound, the bladder needs to be filled. If an examination is carried out for residual urine, then after examining the shape, volume, and structure of the bladder, the patient urinates, and the doctor examines how much urine remains in the bladder. The normal value is no more than 50 ml. There are no contraindications for examining the bladder using ultrasound.
What can replace ultrasound?
If the diagnosis turns out to be uninformative, you can resort to an alternative method - MRI. Diagnostics is based on the principle of nuclear resonance. During the examination, the patient is inside the tomograph.
You must first ensure that there are no possible contraindications. Diagnostics is not carried out if:
- body weight from 120 kg;
- fear of closed spaces;
- pacemakers in the body;
- inability to remain still.
As a result of an MRI, the doctor receives a detailed image. The method is used to clarify a questionable diagnosis.
Preparatory activities
Preparation for an ultrasound of the scrotum does not require any special measures. Sometimes before conducting a study you need to prepare psychologically.
To get acquainted with the doctor, you should take with you a referral and/or conclusions of specialists. This is necessary so that the ultrasound diagnostic doctor pays close attention to the possible cause of the disease.
If we are talking about dynamic observation, then when providing previous examination reports, the specialist will evaluate the changes that have occurred, which is important for determining further treatment tactics.
In order for the ultrasound to take place in comfortable conditions, the patient should bring a diaper or a large towel. The diaper is needed to cover the couch and remove gel from the skin after the examination is completed.
Can everything be seen during the study?
Despite the high accuracy of the ultrasound sensor and the provision of a clear picture, the information content of the examination depends on many factors: the location of the problem, the stage of the disease, its characteristics. For example, when using a procedure to look for an undescended testicle, there is a risk that it will not be found because it is located much higher than the area being examined. In this case, the doctor may prescribe additional examinations and tests. In most cases, the effectiveness of ultrasound is high and the data obtained is sufficient to make a diagnosis and draw up a treatment plan.
Indications for the procedure
Ultrasound is usually prescribed by a urologist or surgeon if test results suggest the presence of pathologies, as well as after a visual examination if the patient has complaints of the following nature:
- pain in the scrotum area;
- change in testicular size;
- the appearance of edema;
- inflammation of the lymph nodes;
- compaction in tissues;
- bloody discharge in semen;
- erectile disfunction;
- difficulty conceiving;
- traumatic injuries.
Some of these symptoms are also characteristic of some other diseases, so you may also be recommended to undergo a prostate ultrasound procedure.
If you find yourself with any of the listed symptoms and you need to consult a doctor who performs ultrasound of the scrotum in St. Petersburg or any other specialist, contact a medical specialist - write to us or call +7 (812) 273-21-85. We will select a convenient time for your appointment and answer any of your questions.
In addition, examination of the scrotal organs is recommended for preventive purposes for adolescents during puberty, men after 45 years of age to monitor health, at any age after urological operations and in preparation for them.