Functions of osteocalcin
Osteocalcin performs a number of specific functions.
These include:
- Formation of bone structures due to osteogenic regulation of metabolism,
- Bone mineralization
- Maintaining an optimal level of calcium, which takes part in osteosynthesis,
- Stimulation of insulin secretion through a direct effect on Langerhans cells (pancreatic cells),
- Increased levels of adiponectin (a hormone) that is released from fat cells.
Bone tissue remodeling. Osteoclasts remove old bone tissue, osteoblasts form new one, releasing the protein osteocalcin, which then enters the bloodstream
Why do you need to get tested for osteocalcin?
Studies of protein content reflect the rate of formation of new tissue, since when it is destroyed (resorption), it is not released. If it is normal, then the processes of osteosynthesis and osteoresorption are balanced, and new tissue is formed in place of dead tissue. At a low level, as well as at an excessively high level, destruction predominates.
Bone Formation Process
Regulation of osteocalcin levels
Hormones that regulate the synthesis of osteocalcin contain calcium: calciferol (vitamin D), calcitonin - a thyroid hormone, parathyroid hormone and parathyrin - hormones produced by the parathyroid glands.
The mechanism of action of calcitonin is to increase the level of calcium entering the inert tissue from the bloodstream, as a result of which the destruction and demineralization of bones is inhibited.
Parathyroid hormone is a calcitonin antagonist, that is, its mechanism of action is the opposite of the thyroid hormone.
Parathyroid hormone helps reduce calcium levels in bone tissue. Calciferol acts on the production of the precursor osteocalcin by osteoblasts.
If the ratio between the amount of calcium produced or calcium-containing hormones is disrupted, this indicates the beginning of the development of bone tissue pathology.
However, what is it?
formation of the active form of osteocalcin
Osteocalcin (OC) is a vitamin K-dependent, non-collagenous protein that is formed by young bone tissue cells that have reached their own maturity - osteoblasts, and is mainly contained in the intercellular substance (matrix), also produced by osteoblasts, where it acts as the main protein that binds calcium with hydroxyapatites. However, a certain amount of this protein (≈10%) is still released from the matrix, leaves its usual location and enters the bloodstream. This care occurs with the participation of vitamin K, which interacts between calcium and calciferol (vitamin D) and large multinucleated macrophage cells (osteoclasts), which dissolve the mineral component of bones and destroy collagen. Osteocalcin, freed from the intercellular substance, representing the remains of γ-carboxyglutamic acid, will subsequently leave the body through the kidneys.
The intensity of production of the described protein is directly influenced by calcium-regulating hormones (thyroid hormone - calcitonin, parathyroid hormone - parathyrin or parathyroid hormone) and calciferol (Vit D). Calcitriol ([1,25(OH)2D3] - a metabolite of vitamin D) stimulates the production of GLA-protein in the cells it synthesizes (osteoblasts) and thereby helps to increase its content in the blood. When the metabolic activity of these cells is disrupted, the concentration of osteocalcin in the blood deviates from the norm, which indicates a certain pathological process.
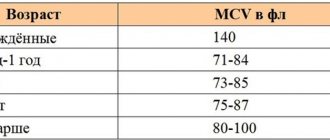
Normal levels of osteocalcin in the blood
The normal range for one bone marker varies depending on age and gender. Also, its indicators may change in women, taking into account the phase of the menstrual cycle. A couple of days before the onset of menstruation, osteocalcin is moderately increased.
During pregnancy, this protein is reduced. In adolescents, this indicator also exceeds the norm due to physiological characteristics.
Age category; Normal levels of osteocalcin in the blood, ng/ml
| Female | Male | |
| 6 months-6 years | 44-130 | 29-121 |
| 7-9 years | 73-206 | 66-182 |
| 10-12 years | 77-262 | 85-232 |
| 13-15 years old | 33-222 | 70-336 |
| 16-17 years old | 24-99 | 43-237 |
| 18-30 years old | 01.11.1943 | 24-70 |
| 30-50 years | 01.11.1943 | 14-42 |
| Over 50 years old | 15-46 | 14-46 |
What factors can affect the results of the analysis?
There are several reasons that may affect the analysis performance:
- In a patient with renal failure.
- In women during menstruation.
These reasons should be taken into account when interpreting laboratory data.
Blood preparation and collection
Hemorrhoids kill the patient in 79% of cases
It is recommended to take Osteocalcin in the morning on an empty stomach. On the eve of the test, you should not abuse alcohol or overeat. The intake of pure still water is not limited. An hour before blood sampling, you must avoid physical and psycho-emotional stress, and smoking. A few milliliters of blood is withdrawn from any peripheral vein into a chilled heparin tube and immediately centrifuged. The biomaterial is placed in ice water and immediately delivered to the laboratory. If necessary, frozen blood can be stored for several months.
There are several known methods for determining osteocalcin in the blood: radioimmunoassay, enzyme-linked immunosorbent assay, one-step chemiluminescent immunoassay based on the “sandwich” principle, specific for intact osteocalcin and fragment. The latter method is currently considered the most common, reliable, fast and sensitive method. Heparinized plasma or serum of the patient is used for the study.
This method is based on the use of two highly specific monoclonal antibodies, one of which recognizes the osteocalcin molecule, and the other - a fragment. During immune reactions, osteocalcin and the fragment are located between two antibodies, as in a “sandwich”. The resulting sample is incubated for an hour. After adding reagents, the sample changes color. Then the optical density of the colored solution is measured with a spectrophotometer. Color saturation is directly proportional to the amount of osteocalcin in the blood. All steps are performed using an automatic chemiluminescence immunoassay analyzer.
What does low osteocalcin in the blood indicate?
Osteocalcin in the body can be reduced as a result of developing pathological processes, among which are the following:
- Rickets in young children,
- Increased amounts of parathyroid hormone, and decreased levels of calcium and calcitonin,
- Itsenko-Cushing syndrome and disease, during which the exchange of hormones in the adrenal cortex is disrupted,
- multiple myeloma,
- Primary biliary cirrhosis,
- Somatotropin levels are below normal,
- Disruption of the parathyroid glands, accompanied by a decrease in its function,
- Decreased calcium levels due to the development of a malignant tumor.
Formation of the active form of osteocalcin
Osteocalcin reduced treatment
Meanwhile, there are circumstances when the level of the described protein in the blood is reduced. During pregnancy, it is lower due to physiological reasons, so such features of the gestational period can be omitted without classifying them as any health problems. A decrease in osteocalcin in the blood also occurs in the following conditions:
- Rickets in young children;
- High concentration of PTH (parathyroid hormone, parathyroid hormone), but low levels of calcium and calcitonin due to the formation of certain pathological processes;
- Hypercortisolism is a syndrome and Itsenko-Cushing's disease, and the more severe the symptoms, the lower the level of osteocalcin observed in the blood;
- Generalized plasmacytoma (myeloma);
- Primary biliary cirrhosis;
- Insufficient production of somatotropin (GH);
- Hypofunction of the parathyroid glands.
In addition to the above reasons, the use of glucocorticoids can reduce the concentration of GLA protein.
Decreased bone density is a virtually asymptomatic disease in the early stages. The main task of an orthopedic traumatologist in diagnosing osteoporosis is to objectively assess the patient’s condition. The specialist identifies the fact of pathology, finds the cause of the disease and differentiates bone loss from other similar or concomitant diseases, and makes a prognosis for recovery.
At the doctor's disposal:
- possibility of clinical examination;
- hardware diagnostics (X-ray, ultrasound);
- laboratory diagnostics;
- genetic examination methods.
All of them are aimed at visualizing macro- and microarchitecture and identifying processes leading to a decrease in bone mineral density.
Clinical examination
At the clinical examination stage, the therapist can identify a group with an increased risk of osteoporosis. Among the symptoms of osteoporosis, the doctor can identify kyphotic deformation in the thoracic spine, a noticeable decrease in the patient’s height compared to the previous visit. Clinical markers of osteoporosis also include complaints of back pain. There is a chance to get an appointment with a traumatologist:
- in women with premature menopause;
- in people with a family history of osteoporosis;
- with frequent fractures under the age of 45;
- in patients with diseases that provoke secondary osteoporosis;
- after taking a number of pharmaceutical drugs;
- with extreme thinness – anorexia, exhaustion, congenital thinness with a BMI less than 20.
If a person has two or more risk factors, the likelihood of osteoporosis increases by a third, regardless of age.
Interviewing the client can help identify additional risk factors:
- calcium deficiency in food;
- lack of exposure to sunlight, and therefore a lack of vitamin D;
- problems with the stomach and intestines;
- drinking alcohol and smoking;
- treatment with glucocorticoids or hormones;
- diseases of the glands and internal organs, COPD;
- prolonged immobilization or low physical activity.
2. X-ray signs of AP
3. Persons over 65 years of age with decreased height or thoracic kyphosis
2. Corsets, thigh protectors
3. For back pain, limit the amount of time you sit
4. Combined calcium and vitamin D preparations
5. Antiresorptive drugs (HRT, bisphosphonates, calcitonin, strontium ranelate)
2. Persons taking glucocorticosteroids for a long time
3. Combination of several risk factors over the age of 50 years
5. The doctor’s decision to prescribe antiresorptive drugs (HRT, bisphosphonates, calcitonin, strontium ranelate)
2. The presence of somatic or other pathology that is potentially dangerous for the development of AP
3. Hypogonadism (including menopausal women)
4. Insufficient calcium intake
Patients with suspected osteopenia or osteoporosis are prescribed further in-depth examination. Often the disease is detected at a late stage by traumatologists in patients with fractures or neurologists in patients with pain in the spine.
An orthopedic traumatologist or neurologist differentiates osteoporosis from bone cancer, trauma, osteomalacia, fibrous dysplasia, Paget's disease, and peripheral neuropathy. Laboratory diagnostics becomes the main basis for decision-making in this case.
The following “clinical myths” serve as an obstacle to early detection of the disease:
• in COPD, osteopenia occurs in more than 40% of patients, and when taking systemic glucocorticosteroids, the frequency of osteopenia reaches 85%;
• in CVD, osteopenia is observed in more than 68% of cases, and AP is diagnosed in 50% of cases
Diagnostic methods
More than 70% of bone strength is provided by mineral density (BMD), the remaining 30% is redistributed between mineralization, metabolism, macro- and microstructure, and microdamage. It is important to identify all defects in the early stages of the disease. For this purpose, a number of methods for diagnosing osteoporosis have been developed.
Most often, osteopenia and osteoporosis are detected using conventional x-rays in the presence of bone fractures or spinal deformities. At this stage, more than a third of bone mass has already been lost. You can influence the process when we are talking about losses of up to 5%. Therefore, for the early detection of osteoporosis, there are more accurate methods:
- ultrasonic;
- isotope (mono- and biphoton absorptiometry);
- mono- and bioenergetic absorptiometry (DXA);
- quantitative computed tomography;
- blood chemistry;
- genetic studies of materials.
Rules for formulating the diagnosis of AP
Ultrasound
Analysis of the mineral composition of bones using ultrasound can identify areas of reduced density. This test for osteoporosis is based on the reflection of ultrasound beams from dense organs. The introduction of ultrasound devices into clinical practice makes it possible to assess the mechanical properties of bone tissue. Strength and elasticity create a hyperechoic image structure.
The testing site for ultrasonic densitometry (UD) is usually the heel bone and the tip of the index finger. Practice shows that this study is more suitable for screening. It is recommended to undergo it once every 5 years for early detection of the problem for women over 45 years of age and men over 50.
Radiodensitometry
An accurate diagnosis is established by examining certain areas of the skeleton using bioenergetic absorptiometry, which is considered the “gold standard” for diagnosing osteoporosis. Dual-energy X-ray absorptiometry aims to measure BMD. Diagnosis is carried out for the entire skeleton, vertebrae, paired sections or one bone. The device compares the received image with the reference ones and produces two indicators, T and Z.
The T-index indicates deviations from the peak bone density of an adult, and the Z-index indicates deviations from the norm for a given age. Normally T=1. Osteopenia is diagnosed at T from -1 to -2.5, lower mineral density is classified as osteoporosis. If the patient has a history of a fracture with a T less than -2.5, then osteoporosis is called severe.
Bone loss affects the entire human skeleton, although unevenly. BMD is determined in places where fractures occur most often. This:
- lumbar vertebrae;
- femoral neck;
- distal forearm.
Postmenopausal women will likely have their vertebrae assessed, while older adults (over 65 years) will likely have their proximal femoral BMD measured. DXA is prescribed for the initial diagnosis of osteoporosis and evaluation of the effectiveness of therapy. The examination is repeated after a year.
The examination is not dangerous to health, since the radiation intensity is 400 times less than with a regular x-ray. The only contraindication may be pregnancy.
DXA does not require any special preparation. It is better not to take calcium supplements the day before. The physician is informed of recent barium examinations. After scanning the selected area, the patient receives images and a conclusion.
The DXA method has some limitations, which are compensated for by additional research.
CT densitometry
Using computed tomography, it is possible to determine reduced tissue density and obtain a three-dimensional image of the anatomical structure of a skeletal area. The study allows us to study the trabecular structure of the bone.
For examination using computed tomography, a peripheral scanner with a thin beam is used to determine the mineral composition of the tissue. The analysis is called CT densitometry and allows you to determine local changes in mineral composition.
Magnetic resonance imaging was discovered in 1946. The study makes it possible to obtain a three-dimensional image of organs by recording a radio signal, which is obtained due to the vibration of hydrogen atoms of aqueous tissues in a magnetic field. For this discovery, scientists received the Nobel Prize.
MRI is rarely used to diagnose diseases, although its possibilities are endless. The analysis allows you to see the trabeculae of the bones very clearly. This property was used to create densitometers - devices for determining the degree of osteoporosis.
Single publications in the literature indicate the high effectiveness of the study in determining the density of the bone structure. Obviously, MRI can be used to check the structure of organs. However, the test is rarely used due to the high cost of the procedure.
The causes of bone loss, like osteoporosis itself, are not obvious. To identify them, you will need to conduct a biochemical blood test and genetic tissue studies. The first one is needed for:
- carrying out preventive measures in cases with metabolic disorders of bone tissue remodeling and resorption;
- predicting the rate of bone loss;
- assessing the effectiveness of therapeutic methods.
At this stage of diagnosing osteoporosis, osteomalacia, bone metastases, and hereditary diseases are excluded, the causes of secondary osteoporosis are identified, and metabolic features are established.
In this case, doctors use three groups of biochemical markers of pathology:
- Markers of bone tissue formation.
50 years –ng/ml.
50 years –ng/ml
inhibits the activity of osteoclasts and thereby bone resorption;
CT densitometry
What are the reasons for increased osteocalcin in the body?
An increase in osteocalcin in a blood test can be caused by the following conditions:
- Accelerated metabolism in bone tissue structures,
- For osteoporosis during the postmenopausal period,
- Chronic renal failure, which leads to nephrogenic osteodystrophy and calcium metabolism disorders,
- Paget's disease
- Fractures of bone structures,
- Disorders of the thyroid gland, in which the level of hormone activity increases - primary hyperthyroidism (toxic goiter, Graves' disease) and secondary changes due to tumor processes in the pituitary gland,
- Pituitary pathologies, in which there is excessive synthesis of somatotropic hormone,
- Malignant formations of bone tissue,
- Osteomalacia – decreased level of bone mineralization,
- Taking medications that contain calciferol and its producers, vitamin B7, as well as medications against epilepsy.
Possible diseases
The immediate causes of deviations from the norm in the analysis are provoked by pathologies:
- Hypoparathyroidism. With this disease, the main emphasis in treatment is aimed at stabilizing and then normalizing the levels of calcium and phosphorus in the blood. Hypoparathyroidism is characterized by a deficiency of parathyroid hormone, a hormone produced by the parathyroid glands. The clinical picture of this condition boils down to hormonal imbalances associated with excess levels of calcium and phosphorus in the blood.
- Hypofunction of the thyroid gland. A decrease in the functions of the thyroid gland in the production of the most important hormone - thyrocalcitonin - provokes the development of osteoporosis, arthritis and other joint pathologies. Deficiency of thyrocalcitonin also leads to diseases of the cardiovascular system. If the level of the hormone decreases to the maximum level, then the process of leaching calcium from bone tissue begins, which leads to disruption of the functioning of the heart and blood vessels.
- Liver failure (biliary cirrhosis). Liver failure is a serious pathological condition. A syndrome that is accompanied by damage to liver cells and organ dysfunction. The liver loses its compensatory capabilities and partially loses its basic functions. The patient exhibits symptoms of chronic intoxication. Progressive biliary cirrhosis can cause hepatic coma, that is, complete organ failure and extensive damage to all body systems, including the brain, by decay products.
- Osteoporosis and atherosclerosis. The rate of development of pathologies and the level of metabolism in bone tissues and blood vessels are determined by the amount of bone protein in the patient’s body. In the early stages of the disease, the indicators will be normal, but with severe metabolic disorders they will increase several times.
In this case, it is necessary to identify pathologies of the thyroid gland and diagnose osteoporosis by resorting to other research methods.
Osteoporosis – what is it?
Osteoporosis is a chronic bone disease accompanied by an increased level of bone fragility due to a deficiency of calcium ions. With osteoporosis, the following symptoms are distinguished: general weakness, night cramps, periodontitis, lower back pain, fragility and splitting of nails.
Among the risk factors for the development of osteoporosis are hereditary factors, older people, female gender, a sedentary lifestyle, and hormonal disorders.
Osteoporosis can be diagnosed in women during menopause.
This is explained by the fact that until this moment, female sex hormones, estrogens, were actively acting on the bones, the amount of which decreases in the postmenopausal period.
What is the connection between osteoporosis and the formation of atherosclerotic plaques?
It is worth paying attention to the fact that atherosclerosis and osteoporosis have many similarities in their etiology, pathogenesis, development, consequences, namely:
- These diseases are typical for people in the older age group.
- The initial stages are asymptomatic.
- The same risk factors: smoking, physical inactivity, low estrogen levels.
- The pathophysiology of the development of both pathological processes is a violation of calcium metabolism.
- The same hormonal regulation and disorders that are characteristic of osteoporosis and atherosclerosis.
- Therapeutic drugs prescribed for osteoporosis have a beneficial effect on the vascular system, and anti-atherosclerotic drugs can help with bone diseases.
Osteoporosis
Diagnosis of osteoporosis
The main diagnostic test for osteoporosis is a blood test for osteocalcin, which can be prescribed in different cases: to diagnose rickets in children, with hypercalcemic syndrome, to study the effectiveness of drug treatment of osteoporosis, for women during menopause.
To collect the analysis, venous blood is taken. The day before the test, you should not eat fried or fatty foods, and you should not drink alcoholic beverages.
You should also not engage in excessive physical activity. Blood is donated on an empty stomach; the patient must not eat for at least eight hours. Before this, instrumental research methods are prescribed: ultrasound, radiography.
There are also other markers of osteoporosis, tests for which are necessary to diagnose this disease:
- Alkaline phosphatase, which plays an important role in phosphorus-calcium metabolism,
- Ionized calcium,
- Calcium and phosphorus in daily urine,
- Calcitonin,
- Parathyroid hormone,
- Somatotropic hormone,
- Beta crosslapse is a marker of bone resorption,
- Serum osteopontin,
- Deoxyproline is an indicator of bone metabolism that is found in urine.
- Tests for women include checking estrogen levels.
You can take the necessary tests in the Invitro laboratory.
Osteoporosis interpretation of the results of these tests is carried out only by a doctor.
Osteoporosis and its relationship with atherosclerosis
Osteoporosis is directly related to metabolic disorders of bone tissue. However, it is known that these disorders are more often observed in women - their bone strength is naturally lower. And, if during reproductive age estrogens are taken to protect the female skeletal system, then with the onset of menopause, due to a decrease in their level, they lose the ability to cope with this task.
Probably, many patients have already noticed that pathological conditions such as osteoporosis and the formation of atherosclerotic plaques on the walls of blood vessels run parallel to each other. So what connection does a progressive decrease in bone tissue mass, disruption of its microarchitecture, and increased catabolism in bones have with atherosclerosis? And here's what:
- The risk of both diseases correlates very markedly with age (the lowest risk is observed in young healthy people);
- Absence of clinical manifestations in the initial period of the disease (neither osteoporosis nor atherosclerosis at first indicate symptoms of the disease);
- Both pathologies create a high degree of likelihood of developing complications of diseases of the cardiovascular system, as well as the occurrence of fractures with the slightest injury in postmenopausal females;
- Their risk factors are, in principle, the same - bad habits (mainly smoking), a sedentary lifestyle, a lack of estrogen, which protect women before menopause;
- The pathophysiological basis of these pathological conditions is also the same - calcium metabolism disorder;
- Disorders of the functions of hormonal systems that regulate calcium metabolism also go in the same direction;
- Many medications intended to treat atherosclerosis are useful for osteoporosis (help maintain bone mineral density), and medications aimed at combating osteoporosis have a beneficial effect on the condition of blood vessels.
Osteoporosis, which increases the level of osteocalcin in the blood, has such a connection with atherosclerosis.
What drug treatment should be prescribed?
Therapeutic therapy for osteoporosis includes different groups of drugs that need to be purchased after a doctor’s prescription.
Among them are estrogens for women, which act effectively and subsequently eliminate the need for a woman to ask the question of how to increase the level of female hormones.
Selective estrogen receptor modulators, calcium-containing drugs, and bisphosphonates are also prescribed.