First aid
The speed of recovery and the number of complications that develop depend on whether first aid was provided to the victim. The person should be immediately placed on a hard surface and the injured shoulder should be kept at rest. This can be achieved by positioning the arm in an abducted position - the elbow needs to be slightly bent and a cushion or folded cloth placed under it. A bandage to support the upper limb in the abducted position will allow the joint to be completely fixed. This is a triangular scarf, in the middle of which the forearm is placed, and the ends are tied with a knot at the back of the neck. In addition to immobilizing the hand, the main task of first aid is to improve the well-being of the victim. What can be done to reduce the severity of pain:
- Apply an ice pack wrapped in thick cloth to your shoulder to prevent frostbite. The maximum time for applying a cold compress is 15 minutes every hour. The procedure not only helps eliminate pain, but also prevents the spread of inflammatory swelling to healthy joint structures;
A cold compress and immobilization of the affected arm are first aid measures.
- give the victim a tablet (1.5 for acute pain) of any anti-inflammatory non-steroidal drug - Diclofenac, Nimesulide, Ibuprofen, Nise, Ketorol. You can also dilute a Nimesil sachet in 100 ml of water.
In case of acute pain, you must call an ambulance. This is a characteristic symptom of combined joint damage, so the victim is hospitalized for examination and surgery. If a person complains of mild or moderate pain, then immediately after fixing the arm, he should be taken to the emergency room for realignment of the shoulder joint.
Habitual dislocation of the shoulder joint: injection of anesthetic before reduction.
Indications for use
In clinical surgery, orthopedics, neurology and therapy, various pathologies of the shoulder joint are quite common. As a rule, patients turn to specialists with complaints of pain, deterioration of joint mobility, severe swelling, and concomitant neurological phenomena.
The following diseases can be the sources of such conditions:
- traumatic injuries (fractures, dislocations);
- inflammatory diseases;
- degenerative-dystrophic processes;
- pathologies of blood vessels or nerves;
- the presence of metastases in the joint structures.
For each of the numerous pathologies, a quick and correct diagnosis is necessary, which can accurately show which structures of the shoulder joint are damaged, by what process and what is the severity of these damages.
Examination of the patient, collection of all complaints and medical history provide, of course, a huge amount of information, on the basis of which the doctor makes a preliminary diagnosis. But many pathologies have similar symptoms and course characteristics, so they need to be quickly differentiated, that is, to exclude the presence of some diseases and to clarify one that is actually present in a particular patient.
For this, various methods of additional diagnostics are needed. The most important role is played by laboratory methods that study blood, urine and other biological media of the body, which reflect the reaction of internal organs and systems to negative changes in the shoulder joint. But there are ways that allow you to see “with your own eyes” what kind of disease is “nesting” in it, how it has changed and continues to disrupt its structure, and also to note how effective the prescribed treatment is and at what rate the recovery process is occurring.
These methods include, first of all, the x-ray method, which can be called the most traditional and time-tested, in demand and affordable. It is necessary to take an X-ray for almost all pathologies of the shoulder joint; this method helps doctors obtain maximum diagnostic information and prescribe timely and competent therapy.
Folk remedies for ankle sprains
If you have a sprained ankle, you can use proven traditional medicine recipes. They will help get rid of excessive swelling, pain and hematomas at the site of injury:
- Compress of 5 grams of salt and 100 grams of 9% vinegar;
- Lotions from tincture of celandine, calendula, string and tansy;
- You can make an ointment that consists of camphor powder, ammonia, a small amount of laundry soap, lamp oil and turpentine.
Instead of getting such an injury, it is better to prevent it. To do this, you must not overdo it with physical activity. Your diet should include foods that contain large amounts of calcium. You can compensate for the deficiency of this microelement by taking special vitamin supplements.
If you have problems with your feet (for example, flat feet), you must wear special shoes with orthopedic characteristics. Only in this case can the risk of ankle sprain be reduced.
Can an X-ray show a herniated disc?
Doctors Skoromets and Zadvorny developed radiological factors for detecting pathologies of the spinal column. They become a reason for additional diagnostic procedures.
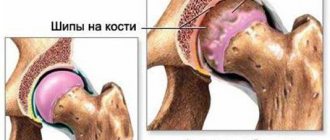
- If an x-ray revealed a straightening of the physiological curve of the spine forward (lordosis), while on some cervical vertebrae the semilunar processes are sharpened, and the apices are sclerotized, the intervertebral space has become shorter - these changes indicate various diseases of the musculoskeletal system - from hernia to osteochondrosis.
- The second stage of the disease has arrived – osteosclerosis of the subchondral type is visible. Dystrophic and degenerative processes lead to the destruction of the fibrous ring and loss of the nucleus pulposus. Growths are noted along the edges of the lateral or anterior bodies of the affected vertebrae.
- The third stage is with a strongly narrowed intervertebral space and bone osteophytes. The vertebral fissure takes on a wedge-shaped shape. When examining the cervical spine, many semilunar processes are found.
If an intervertebral hernia is combined with deforming spondylosis, the signs of the disease are clearly pronounced. The patient's suffering can be temporarily alleviated with the help of non-steroidal anti-inflammatory drugs (NSAIDs).
The presence of beak-shaped vertical growths in the image is a sign not only of degeneration of cartilage and bone tissue. This often happens with spondylosis, when the spinal ligaments become calcified. Differential diagnosis with osteochondrosis is made based on the height of the intervertebral space. In patients with spondylosis it remains the same.
It is also important to distinguish this condition from fixing ligamentosis (Forestier disease) and ankylosing spondylitis.
Before the x-ray, the patient is faced with the clinical picture of the pathology. The x-ray shows a violation of the physiological curves. If the hernia is located in the chest or thoraco-abdominal diaphragm, the patient is diagnosed with kyphosis.
If an x-ray shows the presence of osteoporosis, such a condition may indicate various pathologies of the spinal column. Thinning vertebral bodies are a sign of malnutrition of the vertebrae. This happens with degenerative processes and hernia.
An X-ray indicates indirect signs of dystrophy and degenerative processes. We are talking about osteosclerosis and osteoporosis, characteristic of many pathologies of the spine that affect soft tissues and bones.
During the examination, a Schmorl's hernia can be detected. In this case, the nucleus pulposus penetrates the bodies of nearby vertebrae. As a result, the endplates of nearby segments also bend.
Educational medical literature, online library for students in universities and for medical workers
Recognition of dislocations using conventional clinical examination methods is quite reliable.
Only in rare cases are dislocations seen or mistaken for fractures, especially when the peripheral parts of the extremities are damaged. Therefore, in most ordinary everyday cases there is no need to resort to x-ray assistance, and the radiologist relatively rarely has to see dislocations in large joints. X-ray examination of dislocations, like the examination of fractures, is the most accurate and has a decisive diagnostic value; it is indispensable in every controversial or more difficult case for the clinician. X-rays bring clarity to topographic relationships, detect all sorts of unexpected frequent complications, as well as obstacles to reduction, serve as the most reliable means of monitoring the results of reduction, etc. A natural disadvantage of X-ray examination is that it is somewhat one-sided: both for fractures and dislocations The radiograph does not say anything directly about the condition of the soft tissues, about the main damage to the bursa, ligamentous apparatus, articular cartilage, nerve and vascular trunks and muscles. Let us recall that a dislocated bone is considered to be peripheral, lying distal to the proximal one, which remains fixed. For the spine, the overlying vertebra is designated as dislocated; when there is a displacement between the base of the skull and the first cervical vertebra, they speak of a dislocation of the head.
The main radiological symptom of dislocation (Fig. 35 and 37) is that the articular surfaces are not adjacent to each other, the normal spatial relationships between the main elements of the joint - the articular head and the socket - are disrupted; The articular cavity appears deserted in the image, and the head of the joint is located away from the cavity. If the articular surfaces do not touch each other at all, and the head has completely moved away from the socket, then the dislocation is designated as complete; subluxation, or incomplete dislocation, is a partial displacement of the head in relation to the cavity while maintaining their partial contact.
To diagnose a dislocation means not only to state the fact of dislocation, but also to accurately indicate the direction of the displacement. Without a topographic characteristic of the displacement, there can be no rational reduction.
Rice. 35. Traumatic fresh dislocation of the right hip in a pilot who fell from a helicopter.
Rice. 36. Traumatic periostitis on the anterior internal surface of the tibia one month after being hit with a stick.
The direction of displacement is noted in anatomical terms defining the position of the distal dislocated bone. Only examination in at least two projections gives a true idea of the direction of the displacement. If the displacement occurred in the plane of the central ray, for example, forward when the shoulder is dislocated, then in the picture in the usual posterior position the head of the humerus may be projected in its normal place, in the glenoid cavity. One single image, therefore, can be a source of diagnostic error here too.
That light strip, which appears as an articular space on an X-ray (the so-called X-ray joint space), is in fact not a projection of the true, anatomical joint space, but a projection in reality in a living person of a non-existent interosseous or interepiphyseal space, which, however, every of us clearly imagines on the basis of the usual picture of a joint on a macerated skeleton. The cartilaginous head and the cartilaginous glenoid cavity, which are directly adjacent to each other, naturally cannot be visible on an x-ray. If the integumentary cartilage is thin, like that of an adult, and has a thickness not exceeding 3-4 mm, then the x-ray joint space is narrow, and the configuration of the head and cavity exactly corresponds to each other. In early childhood, when the extensive epiphyseal sections are not yet ossified, we actually do not see either the head or the articular cavity in the photographs. At best, there is only an image of the ossification nucleus, which in its shape only vaguely resembles the final form of the epiphyseal end in an adult. For this reason, X-ray diagnosis of dislocations in childhood can present certain difficulties.
Recognition is then based on the second radiological symptom of dislocation - the displacement of the axis of the dislocated bone. Since, however, the angle formed by the long bones forming the joint essentially changes all the time under normal conditions, then determining the lateral displacement during a dislocation is not always an easy task. This symptom has, therefore, less evidentiary value than determining the displacement of fragments during fractures. Particularly difficult, as already indicated, is the interpretation of radiographs of the elbow joint.
Traumatic dislocations, at least in a third of all cases, are accompanied by separation of small bony protrusions to which the joint capsule or ligament is attached. When examining large joints, such small fragments may go unnoticed; larger ones are of significant practical interest, and their recognition is one of the most important tasks in the X-ray examination of dislocations. The fact is that they can serve as an obstacle to bone realignment, and then require surgical removal. These are, for example, avulsions of the greater tubercle of the humerus during anterior dislocation of the shoulder, avulsion of the medial epicondyle during external dislocation of the elbow joint, or detachment of a piece of the acetabulum during dislocation of the femur in the hip joint. The separation is almost never absent in cases of dislocation in small joints, such as the interphalangeal joints. This so-called avulsion fracture is easily recognized on radiographs by its isolated bone shadow, which is small in size, has an irregular polygonal configuration and jagged contours. Its localization is especially characteristic - it corresponds to the place of attachment of the ligament or capsule; Opposite the fragment, a defect may be visible on the surface of the epiphysis, the jagged contours of which, the shape and size correspond to the broken piece.
With a habitual dislocation, there is usually a well-defined osteoporosis of the articular ends and the entire distal part of the limb, as well as secondary changes in the joint such as disfiguring osteoarthritis. Atrophy of both the soft and bone parts of the limb is very significant with unreduced chronic dislocations. On the surface of one of the bones, usually the proximal one, at the point of contact with the displaced articular head, a depression may form over time, resembling a new articular cavity. Neoarthrosis develops, which appears in the picture as a real joint with all its radiological signs. A fresh, just reduced uncomplicated dislocation is characterized on the radiograph by a completely normal, unchanged picture.
Causes of ankle injury
Very often, a sedentary lifestyle leads to weakening of muscles and ligaments, and excess weight increases the load on the joints. As a result, all this leads to disruption of the musculoskeletal system. And since the ankle joint is the most problematic part of the body, it most often suffers from various types of damage, including dislocations.
This joint supports the entire weight of the human body during movement. Therefore, with any incorrect or careless position of the lower limbs, it may not withstand the load. The result of this action will be a dislocation of the ankle joint. There are many factors that increase the likelihood of injury:
- moving on uneven surfaces;
- physical activity;
- uncomfortable shoes;
- intense sports training;
- ice;
- walking on wet surfaces;
- diseases of the musculoskeletal system.
Girls who prefer to wear high heels are at risk. When you are in a hurry or walking on slippery or uneven surfaces, your center of gravity may accidentally shift. This will be the result of a twisted foot, and in this case the woman will suffer serious injury. The likelihood of injury increases if the heels are too high and thin, or the girl has no experience wearing such shoes.
It should be taken into account that the legs serve as support for the body. And many people underestimate the importance of healthy feet and ankles. Even the most minor injuries can worsen the patient’s well-being and negatively affect his health. If a person nevertheless gets injured and sprains his ankle, then, based on the symptoms, he is prescribed a reduction and treatment.
Turning of the foot on the inside of the heel when the ankle moves outward can occur due to improper coordination of movement. In this case, tension occurs in the lateral and external ligaments, which greatly complicates the situation.
If, in addition to the characteristic signs of an ankle sprain, a cracking or crunching sound was heard during the injury, then this is an indicator of a ligament rupture or bone fracture. In this case, the lower limb must be immediately immobilized to prevent displacement of the ankle joint.
Typical causes of such damage are the following:
- use of poor quality or uncomfortable shoes;
- congenital foot abnormalities;
- ankle weakness;
- excess weight;
- weakening of ankle ligaments due to frequent injuries;
- excessive physical activity at work or in sports;
- the presence of arthrosis or inflammation in the ankle joint;
- metabolic disorders in the body;
- Frequent rolling of the foot while walking, running, climbing or jumping.
Any of these factors can cause damage to the ankle joint and lead to a sprain or even a fracture.
Anatomy of the elbow joint and types of dislocations
The elbow, like the knee, contains three bones: the humerus, radius and ulna, connected by ligaments that hold them in the correct position. When muscles contract in a joint, the following movements are possible:
- Flexion and extension.
- Rotation.
Near the joint there are nerves and arteries named after the names of the bones.
The structure of the elbow joint
Dislocation can be:
- Full.
- Incomplete (subluxation).
The following types are also distinguished:
- Simple - no fractures or ruptures.
- Complex – accompanied by other injuries to nerves and blood vessels.
Based on the nature of the displacement, dislocations are differentiated into:
- Posterior – develops when the ulna and radius bones are displaced backward. 90% of all dislocations are of this type.
- Anterior - the bones of the forearm move forward.
- Medial - the bones move inward.
- Lateral - the bones move outward.
- Divergent – the bones move in different directions from the joint (inward and outward).
Classification of elbow dislocations
Recovery period
Rehabilitation after conservative treatment
If a person has had a simple dislocation of the elbow joint, recovery after reduction is quick and without any complications. The patient may experience slight restriction of movement in the elbow, especially during extension of the arm. This does not in any way affect the functionality of the affected limb.
After removing the plaster, which is used to immobilize (immobilize) the arm in the elbow joint after realignment for 10–14 days, you need to begin physical therapy. Its goal is to restore normal range of motion and sense of joint position (so-called proprioceptive sensitivity). A traumatologist and physical therapy doctor can help you create an individual rehabilitation program. Full recovery takes 3 to 6 weeks.
Examples of simple exercises you can do at home:
| Target | Exercise |
| Increased range of motion | Flexion and extension of the arm at the elbow |
| Restoring muscle strength around the affected joint | Flexion and extension of the arm with light weight |
| Elbow stretch | While standing, raise your arm in front of your body with your fingers extended. With your healthy arm, bend the hand of the injured limb towards your knees. Hold this position for 5 seconds, then release the hand slowly and with control. |
Some people continue to wear an elbow guard or use an elastic bandage to stabilize the joint and prevent recurrent dislocations.
Until complete recovery, it is better to avoid heavy loads on the joint.
Possible exercises for rehabilitation after dislocation of the elbow joint. 1 – movement on a horizontal surface; 2 – rocking; 3 – use of roller carts; 4 – bending at the elbow with the support of the healthy arm; 5 – rolling a stick; 6 – swinging the stick. Click on photo to enlarge
Rehabilitation after surgical treatment
After surgery, immobilization of the injured arm is also necessary, which is best done with an elbow orthosis. This device allows you to gradually improve mobility in the joint while the soft tissue heals. It helps reduce the formation of scar tissue and minimize the risk of complications.
Elbow brace
After immobilization is eliminated, physical therapy begins, the program of which is helped by a traumatologist or rehabilitation specialist.
A scar at the surgical site may limit movement in the elbow. In addition, there is a certain risk of repeated dislocations. If these problems occur, additional reconstructive surgery may be necessary.
Folk remedies during the recovery period
Many patients in the recovery period begin to use various traditional medicines, trying to speed up rehabilitation. Compresses made from milk, onion, wormwood and propolis are very popular. The effectiveness of these methods raises reasonable doubts among most traumatologists, because the basis for successful rehabilitation after a dislocation is persistent and thorough performance of physical therapy exercises.
How is a shoulder x-ray done?
No preliminary preparation for the procedure is required. Sometimes the patient is diagnosed without even taking off his clothes (if a damaged joint or bone needs to be examined after a traffic accident, but clothes cannot be removed due to a serious injury).
MRI image of the shoulder joint
Once in the X-ray room, the patient must remove his outer clothing (if possible). Be sure to remove any metal accessories from your neck, arms or shoulders.
Next, the patient is placed on a special table; depending on the expected injury, certain positions in which the patient should lie can be assigned. For example, in case of a dislocation, the picture can be taken standing or sitting.
The doctor then places a protective lead apron on the patient. The apron primarily protects the genitals and thyroid gland, since ionizing radiation “hits” these organs the most. If necessary, other organs can be protected (for example, the abdomen, if a pregnant woman is being examined).
Next, the medical staff leaves the X-ray room. The device is started on the control panel; if necessary, through the microphone the doctor can ask the patient to hold his breath.
The procedure in total takes no more than 2-3 minutes, after which the patient can get dressed or go for procedures (if they need to be done urgently, for example after an injury). Test results are usually ready in 15-60 minutes.
Where is the photo taken and how much does it cost?
X-rays are carried out in almost every public medical institution (clinics, hospitals). Rarely, X-ray diagnostic equipment is found in private medical centers.
You can go there or there - there is not much difference, except for the cost. The cost of an X-ray of the shoulder joint (in two projections) in public medical institutions rarely exceeds 800 rubles (on average). The cost of the same procedure in private clinics is 1300-1600 rubles.
X-ray of the scapula and clavicle (video)
How often can I do it?
X-rays of any organ are carried out exactly as many times as necessary. That is, if the patient has a serious illness, and as part of dynamic monitoring it is necessary to undergo an x-ray every day, it must be done every day (naturally, unless the doctor gives other instructions).
The ionizing effect of radiography will be very high in this case, but not enough to seriously harm the patient’s health. Modern medicine has the latest digital equipment for x-ray diagnostics, which creates minimal radiation exposure even with frequent examinations.
Therefore, the procedure can be performed frequently, almost daily for a month (for example). However, in the case of the shoulder joint, there is no disease that would require such frequent radiographic diagnosis.
Maximum - X-ray examinations are prescribed twice a week, for a month or two. This is done for aggressive treatment of arthritis or other inflammatory diseases of the shoulder. In such cases, frequent diagnosis is justified and does not pose a serious threat to the patient’s health.